The spread of COVID-19 has forced healthcare IT into the spotlight. From smartphone-enabled diagnosis to infection tracking, information technology has become central to the fight against the virus. However, COVID-19 response is simply the latest – and most public – example of the rise in digital-health systems. Xtalks checked in with experts on the progress towards digitizing the life-or-death world of medicine.
Anne Snowdon, RN, PhD, Academic Chair of the World Health Innovation Network (WIN) at the University of Windsor, Ontario, Canada, said that healthcare must catch up with the rest of our digital society without delay.
“We can shop online for pretty much anything…we can do almost all of our banking online…we can book any travel. We can even apply for, and get, a passport in this country for 10 years by never meeting a person,” said Dr. Snowdon. “We’re living in a very digital society…except in healthcare.”
“We’ve done incredibly well in solving big, tough issues in curing disease; we have not figured out how to make this system work for people, so that it helps people stay well – and helps people help themselves,” said Dr. Snowdon.
Ajay Sharma is the President of the Central and South Ohio Chapter of the Healthcare Information and Management Systems Society (HIMSS). HIMSS cancelled its international conference last week due to COVID-19.
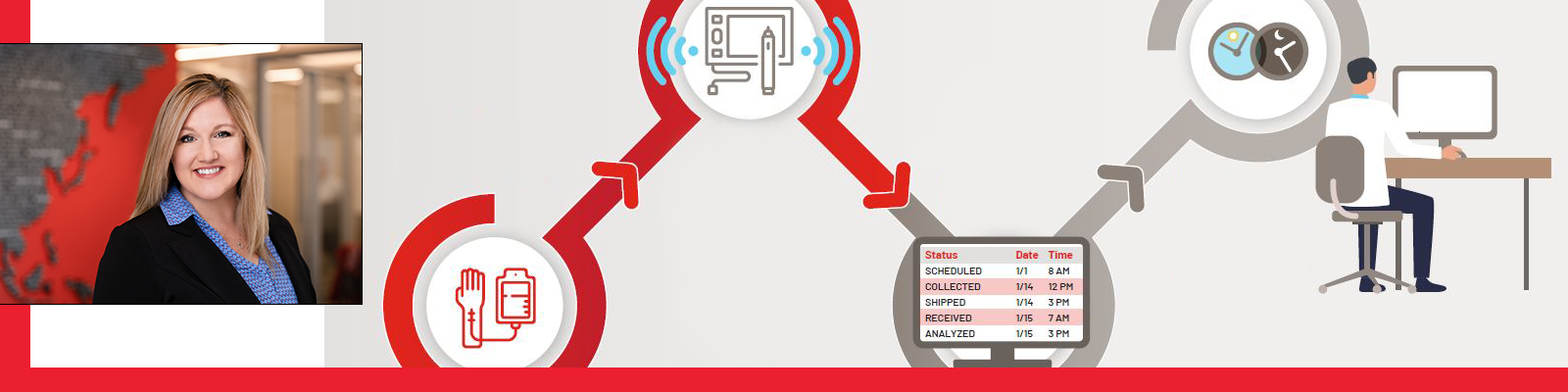
Mr. Sharma highlighted the exciting potential of wearables and smartphones: “Think about the [billions] of people being able to generate health data on a constant basis and how much data is out there.”
The numbers paint the picture. Since the last pandemic, H1N1 flu in 2009, the number of people online has more than doubled to 4.57 billion – almost 60 percent of the world’s population. Mobile devices now account for nearly 70 percent of digital media time and smartphone sales have increased ten-fold, to 1.56 billion a year (see Figure 1).

We have never been in a better position to harness information technology to protect our health, say the experts.
As if to illustrate this, on March 6, the US Government approved an $8.3 billion emergency-response bill that allows Medicare-funded virtual hospital visits using a smartphone during the COVID-19 outbreak. Previously, Medicare only funded telehealth for patients in rural areas.
Mr. Sharma said, “Thirteen years ago, when I got into healthcare, I couldn’t even imagine using a mobile phone to have an e-visit with a doctor… innovation is the key whereby we can use what we currently have to achieve more – to use the same thing, but for a new purpose.”
The Healthcare Ecosystem
Mr. Sharma said healthcare should be viewed as an ecosystem, in which all stakeholders and influencers are interconnected.
The top layer of the healthcare ecosystem is, ideally, global interoperability – a system of patient records that can be accessed anywhere, anytime, in the same way people can get at their money with a bank card from Alaska to Zanzibar.
Although such a set-up is still in the future, the benefits are obvious, said Mr. Sharma, especially in situations such as COVID-19. “How can we ensure a physician can care for a patient travelling to another country just by checking their health records?” he said. “And if we’re able to share information globally we’ll be better able to track global epidemics and pandemics.”
The second layer of the ecosystem is institutional interoperability. This involves connecting electronic health record (EHR) systems within healthcare organizations to improve quality and safety – and save money.
In the US alone, “billions of dollars could be saved if healthcare data were truly interoperable” according to the HIMSS website.
The vision is that a healthcare organization would be able to access data for patients across all their facilities and track trends, outcomes and alerts in real time.
US healthcare executive, George Halvorson, now the CEO of the Institute for InterGroup Understanding, has been an advocate for this approach for 30 years.
“We have crippling silos in all directions,” he explained. “The average Medicare patient in the US has six doctors and they don’t typically communicate with each other.”
As Chair and CEO of managed-care organization Kaiser Permanente for 12 years, Mr. Halvorson implemented a cross-company system that, he said, transformed the organization. Kaiser Permanente currently operates more than 500 medical-care sites and almost 50 hospitals.
Crucially, said Mr. Halvorson, interoperable healthcare systems have the potential to eliminate healthcare disparities. For example, data mining by the Kaiser Permanente team showed that African-American men were more likely to die from prostate cancer – and were less likely to have prostate exams. By standardizing prostate screening, the team was able to reduce prostate-cancer-related deaths. “When you build an algorithm, unconscious bias disappears,” Mr. Halvorson said.
The medical literature now includes many examples where Big Data, increasingly processed by machine learning or artificial intelligence (AI), has improved care.
For example, the University of California San Francisco (UCSF) Medical Center recently validated an AI system called InSight that accurately predicted which patients would develop sepsis (a potentially fatal blood infection) 92 percent of the time. It outperformed the human clinicians, who only got it right 84 percent of the time using standard medical checklists.
To manage such huge data sets, in the last few years hospitals in the US have increasingly offloaded data hosting to cloud providers instead of pouring money into their own data centers, according to Mr. Sharma. “I never thought that so many conservative organizations would move their technology to the Cloud to lower the cost of capital outlay,” Mr. Sharma commented.
The Challenges for Digital Healthcare
Despite such thrilling advances, the full potential of IT in healthcare faces some tough challenges.
At the most basic level, EHR systems are often inadequate for simple day-to-day patient care – never mind sophisticated interoperability.
Edward R. Melnick, MD, and a team from the Yale University School of Medicine in New Haven, Connecticut, published a survey of 5,197 US physicians in November, 2019, that gave EHR systems across the country a failing grade. In the study, which appeared in the Mayo Clinic Proceedings, physicians were more likely to suffer burnout at institutions with poorly designed EHRs.
Another challenge that must be addressed by digital healthcare, said Dr. Snowdon, is the prevalence of medical error. In the US and Canada, medical errors are the third most common cause of death after heart disease and cancer. They are also very expensive to manage and treat.
“We’ve used a lot of checklists but we must get to a more digitally enabled checklist…a digital environment that knows, as I walk into a room I scan a bar code,” Dr. Snowdon said, “so we’re operating on the right person, the right body part, the right drugs, right everything. That’s a digital-environment capacity that we don’t have today in the health system that we absolutely need to get to.”
Privacy is another concern. If we’re sharing health data across institutions, countries and the planet, how do we make the files “eyes only”? To illustrate the challenge, In February this year Google admitted the possibility that employees saw identifiable patient information while moving data from St. Louis-based healthcare provider Ascension into Google Cloud.
Dr. Snowdon said that if other global organizations have figured out privacy, healthcare can too.
“If banking can figure it out, and immigration can figure it out, why can’t healthcare?” said Dr. Snowdon. She concedes that healthcare is more complex than banking, but advocates an approach that “starts with the transactions we all know and understand. Right now, a global network of who’s been vaccinated, and for what, would be really helpful.”











Join or login to leave a comment
JOIN LOGIN