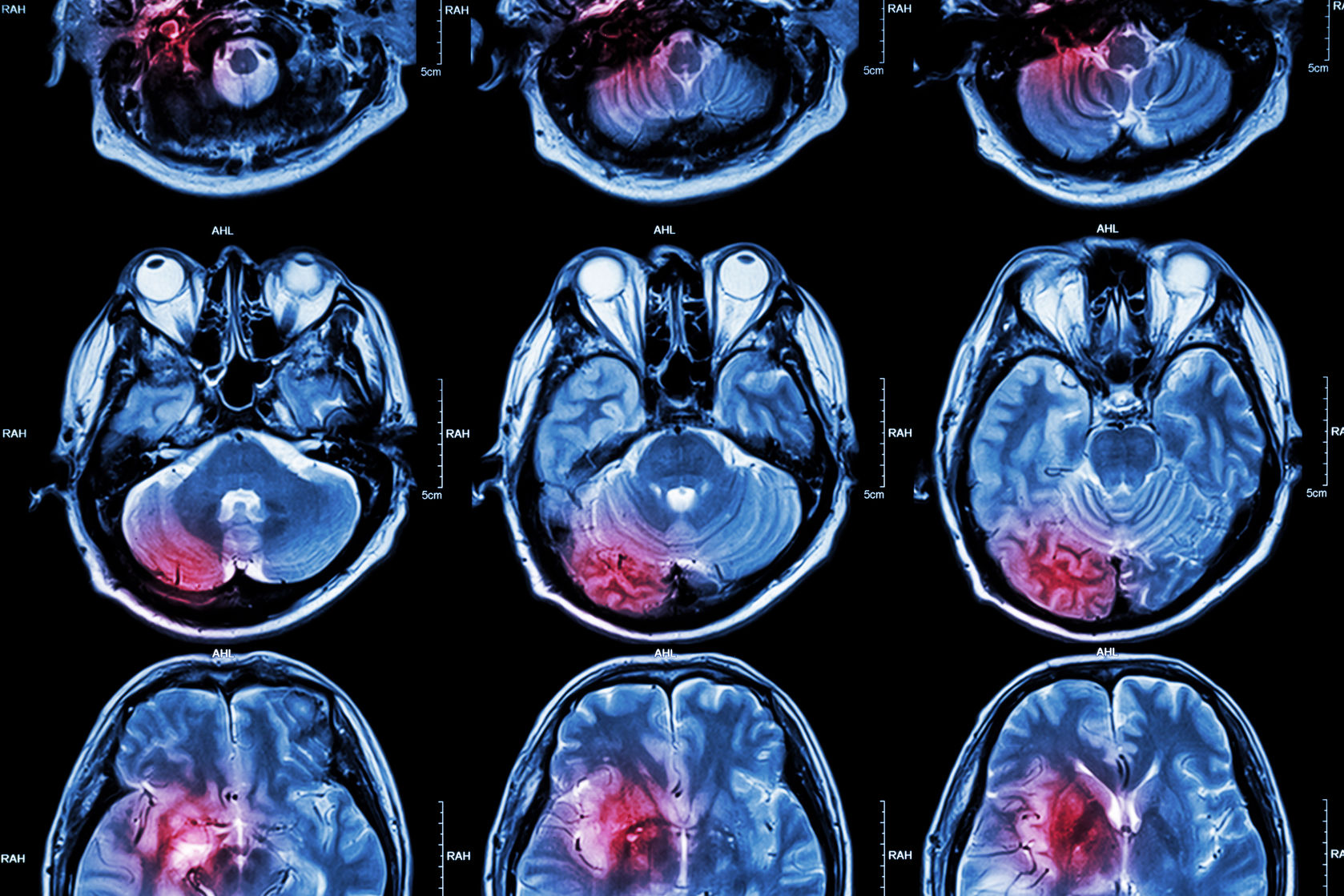
It can be difficult for physicians to identify the underlying cause of heart failure, stroke and other conditions leading patients to receive more general treatment that may not address the root of the issue. Now, researchers at Vanderbilt University Medical Center have developed a method to mine genetic data from electronic health records and identify rare genetic diseases which may be behind a patient’s symptoms.
Among their most important findings in their paper – which was published in the journal Science – was that previously-undiagnosed genetic variants were associated with an increase in transplants. They found that 10 percent of patients with a variant in a gene associated with liver functioning later received a liver transplant, while 14 percent of those with a genetic variant affecting the kidney required a kidney transplant.
According to the researchers, if these genetic abnormalities were identified in clinical practice, patients may have received more tailored treatment which could reduce the need for organ transplants.
“We started with a simple idea: look for a cluster of symptoms and diseases to find an undiagnosed underlying disease,” said Dr. Josh Denny, professor of Biomedical Informatics and Medicine and director of the Center for Precision Medicine. “Then we got really excited when we saw how we could systematize it across thousands of genetic diseases to figure out the impact of millions of genetic variants.”
Using the known features of over 1,200 Mendelian diseases – those with a simple inheritance pattern controlled by one gene – Denny and his colleagues compared this information to symptoms recorded in patients’ electronic health records. They then generated a phenotype risk score for 21,701 patients to predict whether they suffer from an undiagnosed genetic disease.
“What the phenotype risk score shows us is that if you start with specific combinations of symptoms, the chances of finding a potentially causative genetic variant are pretty high,” said co-author Dr. Dan Roden, Senior Vice President for Personalized Medicine. “This is a really important step to using clinical genotyping to assess patient risk and inform more precise prevention and treatment of common conditions.”
In all, the researchers found 18 links between high phenotype risk scores and genetic variants identified in patients’ electronic health records. While two of the variants had been previously identified as those causing cystic fibrosis, the majority of the mutations had not been found to be associated with disease before.
The technique could also help clinicians gain a better understanding of the potential cause of even more complex conditions such as infertility. The research supports a precision medicine approach to treating these diseases and conditions with personalized therapy.
“Phenotype risk scoring can easily be applied in any electronic medical record system that is linked to DNA,” said Bastarache. “Our work looked at only a small sample of the human genome, about 6,000 variants. The opportunity for additional discoveries using this method is huge.”








Join or login to leave a comment
JOIN LOGIN