Three leading medical societies have published new clinical practice guidelines aimed at helping surgeons make more informed choices on the use of anticoagulant drugs during heart procedures. The Society of Thoracic Surgeons (STS), the Society of Cardiovascular Anesthesiologists (SCA), and the American Society of ExtraCorporeal Technology (AmSECT) all collaborated on the guidelines recently published in The Annals of Thoracic Surgery along with two other journals.
“It is our hope that these guidelines will help clinicians practice consistent and safe anticoagulation and that there will be more standardization in practice,” said lead author Dr. Linda Shore-Lesserson, of North Shore University Hospital in Manhasset, NY. “Surgeons, anesthesiologists, and perfusionists will better appreciate the science behind the practices that they conduct every day.”
Cardiothoracic surgeons rely on cardiopulmonary bypass (CPB) to allow them to safely perform their procedures. A CPB pump reroutes blood that would normally make its way through the heart and lungs to an external machine, maintaining artificial heart and lung function while providing surgeons with optimal operating conditions.
However, when blood is exposed to the surfaces that make up the CPB pump, it’s prone to clotting, which could be dangerous for the patient. To combat this, clinicians administer anticoagulant drugs, such as heparin, to thin the blood during the procedure, but reverse the effects of the anticoagulant after surgery using agents such as protamine.
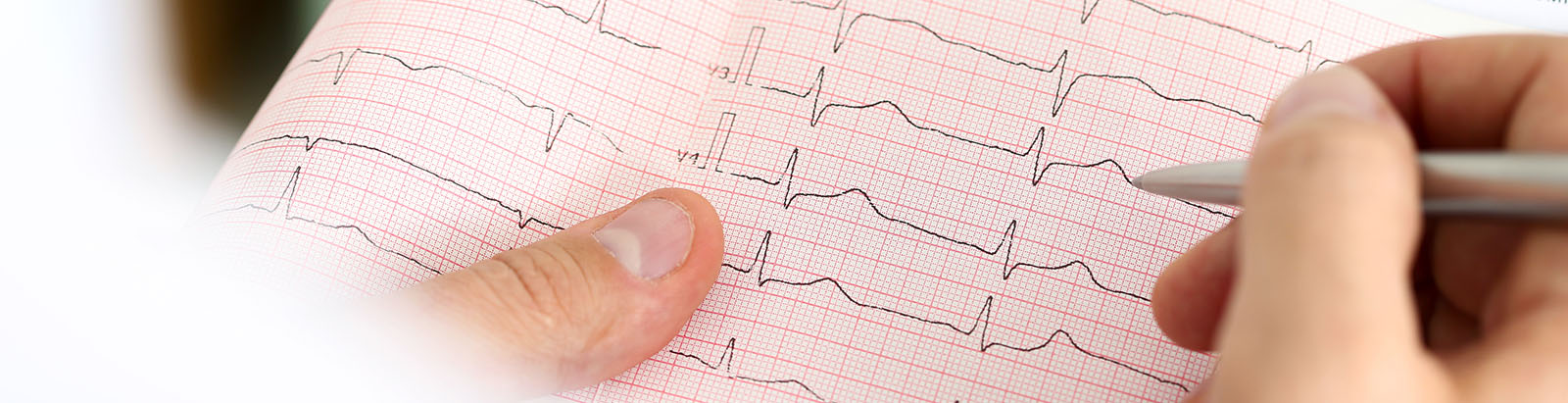
While anticoagulation therapy is widely used during cardiac procedures, a lack of standardization has led to a variety of medication doses being administered to patients. To address this issue, STS, SCA and AmSECT worked together to establish clinical guidelines for the use of anticoagulation therapy during CPB.
“Until now, there has been no standardization of this important practice or the use of these anticoagulant drugs,” said Shore-Lesserson. “These recommendations will help fill the evidence gap and establish best practices in anticoagulation therapy for cardiopulmonary bypass.”
The new recommendations are based on a review of nearly 100 studies. According to Shore-Lesserson, the practice guidelines have the potential to improve patient outcomes following surgical procedures.
“This study examined the relevant existing literature on anticoagulation and its reversal and synthesized cogent recommendations for the clinicians,” said Shore-Lesserson.
Among the new guidelines are recommendations on the initial dosing of heparin, as well as additional doses to maintain anticoagulant status during CPB. Exploring alternatives to heparin if a contraindication is identified, as well as the most effective reversal agents were also topics covered in the guidance.
While heparin and protamine have been extensively used in the last 50 years to modulate the blood’s ability to clot, Shore-Lesserson points out that these drugs could be improved. In order to identify new alternatives to these mainstays, researchers will need to conduct new trials and generate better evidence.
“We hope that this guideline will stimulate investigators to conduct more research and to expand on the evidence base regarding anticoagulation therapy for cardiopulmonary bypass,” said Shore-Lesserson.









Join or login to leave a comment
JOIN LOGIN