Increasing research into the gut microbiome has revealed new and emerging roles for the ‘good bacteria’ in our bodies, with the latest being a new study that shows how they can help the immune system attack cancer cells.
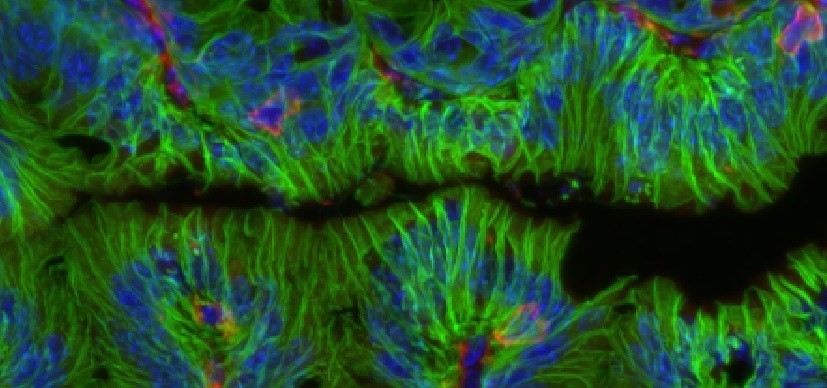
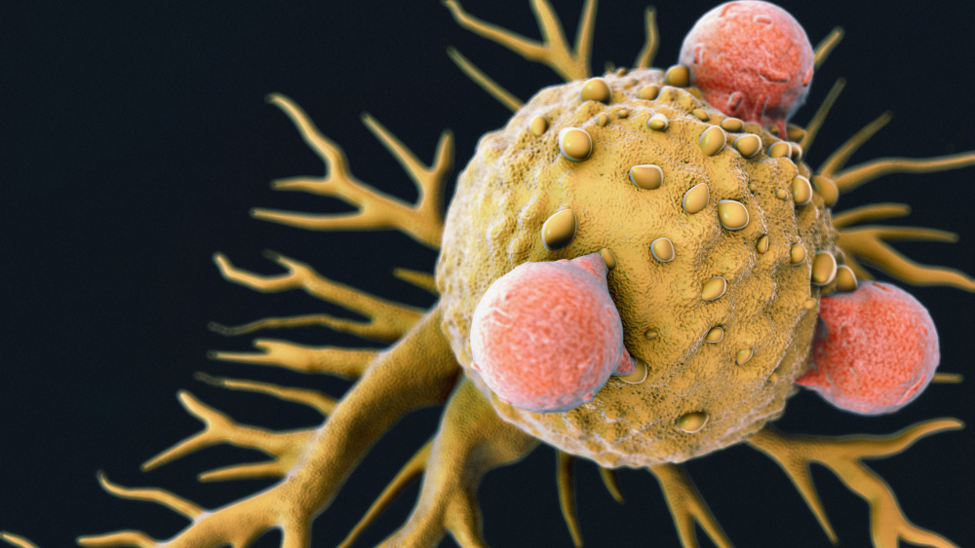
Scientists at the Snyder Institute for Chronic Diseases, Cumming School of Medicine (CSM) at the University of Calgary have learned that certain bacterial species in the gut can enhance immune system responses against cancerous tumours. They discovered that a specific metabolite produced by the bacteria acts on T cells to activate and bolster their action against tumors.
The researchers showed that combining immunotherapy with microbial therapy involving the bacteria effectively shrinks tumors in colorectal and bladder cancer, as well as in some melanomas. The findings were published in the journal Science.
Related: Characterizing the Tumor Microbiome: Bacteria Found in Tumors May Predict Response to Therapy
Commenting on the findings in a press release, Kathy McCoy, PhD, director of the International Microbiome Centre at the University of Calgary and principal investigator on the research said, “Recent studies have provided strong evidence that gut microbiota can positively affect anti-tumour immunity and improve the effectiveness of immunotherapy in treating certain cancers, yet, how the bacteria were able to do this remained elusive.” She said, “We’ve been able to build on that work by showing how certain bacteria enhance the ability of T cells, the body’s immunity soldiers that attack and destroy cancerous cells.”
Specifically, recent studies have shown that several strains of intestinal bacteria improve the efficacy of checkpoint inhibition-based immunotherapy, a type of immune therapy commonly used in cancer treatments, which blocks regulatory signals that shut down immune responses.
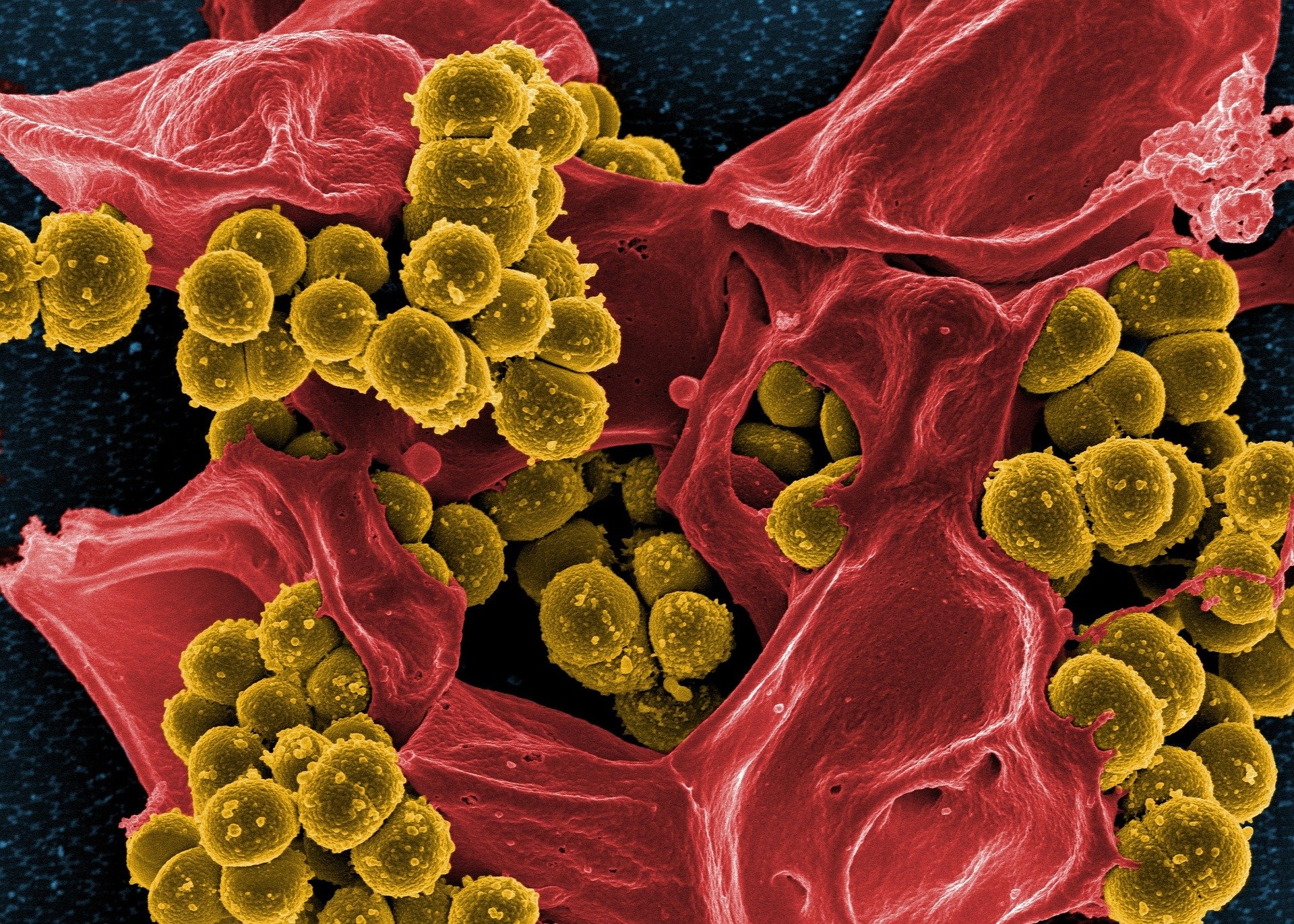
As part of the study, the University of Calgary researchers first identified three different species of intestinal bacteria associated with colorectal tumors: Bifidobacterium pseudolongum, Lactobacillus johnsonii and Olsenella. These bacterial strains were found to significantly enhance the action of immune checkpoint inhibitors in four mouse models of cancer.
In examining the potential mechanisms underlying the activity of the bacteria, the study found that intestinal B. pseudolongum enhanced immunotherapy responses through production of the metabolite inosine, which is a nucleoside (purine) byproduct formed during the breakdown of adenosine; inosine has been shown to have significant immunomodulatory function including powerful anti-inflammatory effects.
Introduction of these specific bacteria, through microbial therapy, in combination with immune checkpoint blockade, led to marked tumor shrinkages. Moreover, the immunotherapy had no effect in mice that did not receive the beneficial bacteria. The immunotherapy decreased gut barrier function, leading to increased systemic translocation of inosine and activation of anti-tumor T cells. Inosine’s effects were dependent on expression of the adenosine A2A receptor on T cells, and required co-stimulation.
“Identifying how microbes improve immunotherapy is crucial to designing therapies with anti-cancer properties, which may include microbials,” said McCoy. “The microbiome is an amazing collection of billions of bacteria that live within and around us everyday. We are in the early stage of fully understanding how we can use this new knowledge to improve efficacy and safety of anti-cancer therapy and improve cancer patient survival and well-being.”
The new research sheds light on mechanisms involved in microbial – immune pathways stimulated by immunotherapies and which can potentially be targeted through microbial-based adjuvant therapies.



Join or login to leave a comment
JOIN LOGIN