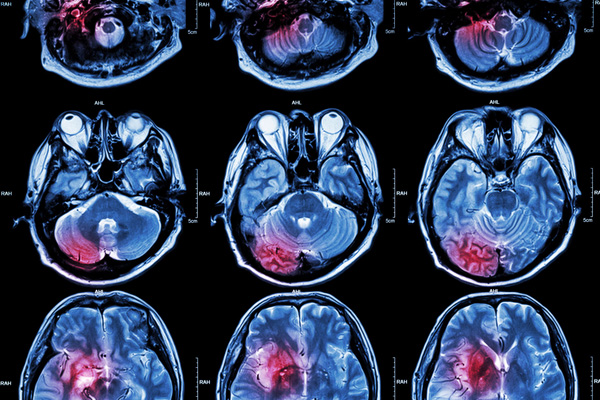
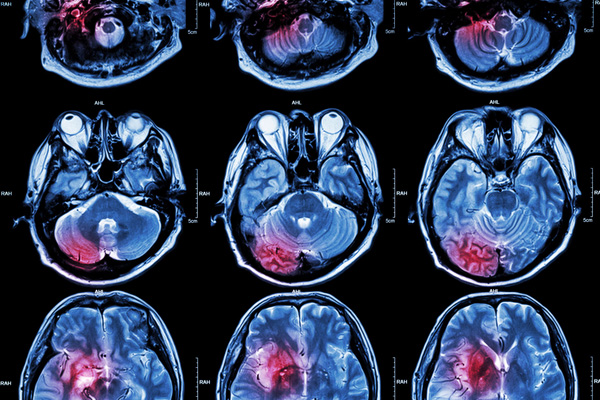
Alzheimer’s disease researchers have long focused on the accumulation of amyloid-beta in the brain as a potential cause of neurodegeneration. But decades of failed trials for therapies targeting this pathway has led researchers at the NYU School of Medicine to propose a new mechanism behind the development of Alzheimer’s.
The study – published in the journal PLOS ONE – suggests that the accumulation of cellular waste products in the brain as a result of a faulty disposal system could trigger the onset of Alzheimer’s. According to the researchers, this process begins decades before cognitive impairment and memory loss occurs.
This incomplete picture of Alzheimer’s disease pathology is a likely contributor to the challenges in drug development for dementia today. As a result of this gap in understanding, currently-available diagnostics are unable to identify the early stages of Alzheimer’s in patients under the age of 70.
Patients diagnosed with Alzheimer’s do display a heightened concentration of one type of amyloid-beta (Aβ42) in their neurons. Combined with the accumulation of another toxic protein, tau, these levels are commonly measured to make predictions about the likelihood of cognitive decline in a given individual. However, the researchers point out that many younger individuals who go on to develop Alzheimer’s disease do not show signs of neural Aβ42 and tau accumulation, suggesting the proteins cannot be the only contributors to the neurodegenerative disease.
“Once you stop assuming that the starting point of Alzheimer disease is marked by the buildup of Aβ42 in brain cells, a different picture emerges,” said lead study author Mony de Leon, EdD, a professor in the Department of Psychiatry, and director of the Center for Brain Health, at NYU Langone Heath. “By recognizing an earlier disease phase, we may be able to start treating earlier and in tailored ways based on a better understanding of disease biology.”
Aβ42 and tau protein levels in the brain are indirectly measured based on their presence in cerebrospinal (CSF) fluid. de Leon and colleagues have been collecting CSF samples from healthy patients through a lumbar puncture procedure since 1999.
Using this clinical database along with two other sources of CSF sample data, the researchers compiled a study size of around 700 patients. While decreased levels of Aβ42 in the CSF were thought to indicate heightened levels in the brain, and therefore a higher risk of developing Alzheimer’s, the researchers found that elevated Aβ42 in the CSF was paradoxically a better predictor of future dementia risk.
By incorporating this information, as well as taking into account the effects of rising tau, the team was able to design a future risk prediction model that was almost 20 percent more accurate when compared to current measures. The current linear risk equation was replaced by a quadratic one to better represent the relationship between Aβ42 and tau levels in the CSF and brain.
This equation was found to be even more accurate at predicting Alzheimer’s risk in people younger than 70. By monitoring tau accumulation over a wider time period, the researchers believe they may have a better picture of Alzheimer’s development compared to just measuring a drop in Aβ42 in the CSF in later life.
Based on their results, de Leon and colleagues propose a “clearance theory” of Alzheimer’s disease. The theory maintains that CSF is pushed through the interstitial spaces between neurons through the pumping action of the heart, which clears cellular waste and potentially toxic proteins from the brain. Cardiovascular disease and other age-related changes in the heart’s ability to function could cause this CSF flow to be weaker, allowing tau to accumulate. However, the study still does not prove causation, leading the research team to wonder whether the true disease-causing protein for Alzheimer’s is still unknown.
“Future CSF studies need to follow normal subjects, starting at age 40, for decades to get an unbiased look at the trajectory of CSF proteins and the likelihood of developing cognitive impairment decades later,” said de Leon.






Join or login to leave a comment
JOIN LOGIN