Sanofi’s pivotal LUNA 3 Phase III study has delivered promising results for rilzabrutinib, marking an important advance for adults living with persistent or chronic immune thrombocytopenia (ITP). ITP is a rare autoimmune disorder that leads to dangerously low platelet counts.
In this study, rilzabrutinib, an oral Bruton’s tyrosine kinase (BTK) inhibitor, demonstrated a durable platelet response in 23 percent of treated patients compared to none on placebo, indicating high statistical significance. These findings position rilzabrutinib as a promising new treatment option for a patient population with limited choices.
Rilzabrutinib joins a wave of innovative ITP therapies, including thrombopoietin-receptor agonists like eltrombopag and romiplostim, which boost platelet production.
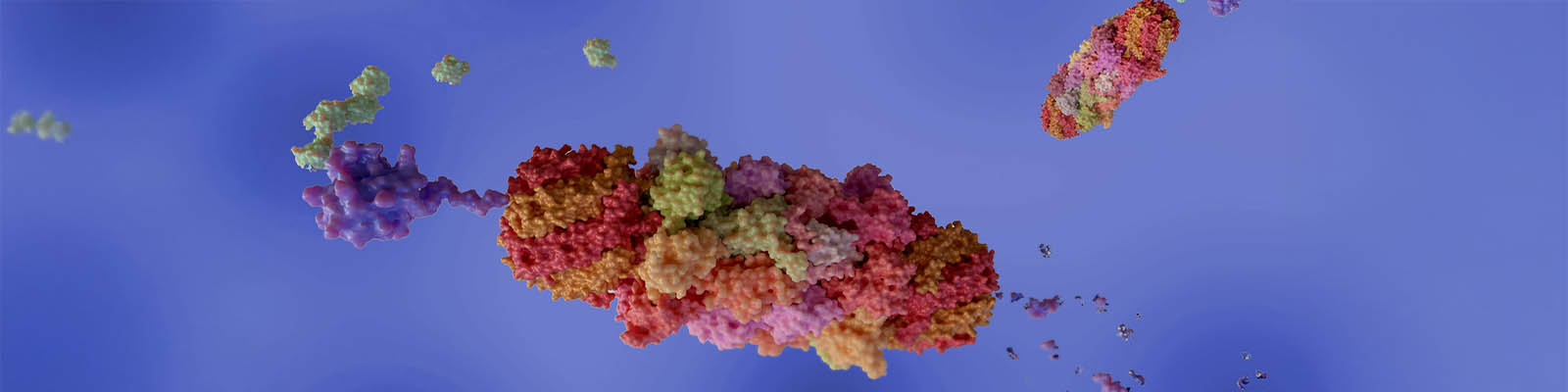
Rilzabrutinib works by targeting BTK, a protein involved in immune cell communication. By inhibiting this protein, the drug disrupts pathways that contribute to platelet destruction and insufficient production. Its selective mechanism aims to minimize off-target effects, making it a potential first-in-class treatment for ITP. Beyond increasing platelet counts, rilzabrutinib also showed reductions in bleeding events and improvements in fatigue, a debilitating symptom that significantly affects quality of life for many patients.
XTALKS WEBINAR: Driving Impact: Change Management Strategies for Clinical Study Design Technology Adoption in Clinical Development
Live and On-Demand: Wednesday, December 18, 2024, at 3pm EST (12pm PST)
Register for this free webinar to learn how to foster alignment across organizations and unlock the full potential of clinical study design technology in clinical development.
The LUNA 3 study enrolled 202 adults with persistent or chronic ITP and severely low platelet counts, averaging just 15,000 per microliter — well below the normal range of 150,000 to 450,000 per microliter. Participants received either rilzabrutinib or placebo for 24 weeks, followed by an open-label extension.
In the trial, platelet response, defined as achieving at least 50,000 platelets per microliter or doubling baseline counts, was seen in 65 percent of patients on rilzabrutinib, compared to 33 percent on placebo. The drug also reduced the need for emergency rescue therapies by 52 percent and delivered significant improvements in patient-reported fatigue scores.
Importantly, rilzabrutinib maintained a favorable safety profile, with most side effects reported as mild or moderate, such as diarrhea and nausea. This aligns with previous studies, reinforcing its potential as a well-tolerated treatment option.
Recent advancements in ITP treatments include CM313, an anti-CD38 monoclonal antibody that achieved a 95.5 percent platelet response in a study published in The New England Journal of Medicine. While promising, CM313 requires intravenous administration, contrasting with rilzabrutinib’s oral dosing and rapid 15-day response.
Another contender, Takeda’s mezagitamab, also targets CD38 and recently earned US Food and Drug Administration (FDA) Fast Track and Orphan Drug designations, with a global Phase III trial planned in 2024.
Rilzabrutinib stands apart by targeting upstream immune pathways through BTK inhibition, offering a distinct approach to managing ITP.
Rilzabrutinib is currently under regulatory review in the US and European Union (EU), with a decision anticipated by August 2025. Ongoing research will also explore rilzabrutinib’s potential in other immune-mediated diseases, underscoring its broader therapeutic possibilities.











Join or login to leave a comment
JOIN LOGIN