The rare disease space is experiencing remarkable growth, propelled by advancements in technology, regulatory incentives such as accelerated approval pathways, heightened funding and investment, robust patient advocacy and collaborative initiatives.
Xtalks spoke with Richard Philipson, MD, Chief Medical Officer (CMO) at Calliditas Therapeutics, a Sweden-based company with full commercial operations in the US focused on developing treatments for rare diseases to learn more about the continuing evolution of rare disease drug development.
Calliditas Therapeutics successfully commercialized its lead candidate targeted release budesonide in the US, where it is known as Tarpeyo, for the treatment of the rare kidney disease immunoglobulin A (IgA) nephropathy. The therapy is the first and only US Food and Drug Administration (FDA)-approved treatment that reduces the loss of kidney function in adults with the disease.
Dr. Philipson, a medical practitioner turned pharmaceutical expert, shared insights into the space of rare disease drug development. He also traced his personal journey from the clinic to leading a rare disease biotech and winning FDA approval for a rare disease drug.
Dr. Philipson’s tenure in general medicine and nephrology provided a solid foundation for his foray into the pharmaceutical industry. Prior to joining Calliditas Therapeutics as CMO, he held roles at GlaxoSmithKline (GSK) and Takeda, focusing on clinical and business development in rare diseases.
“I’ve had a great passion for drug development in rare diseases,” says Dr. Philipson, underscoring a commitment that would shape his career’s trajectory.
Dr. Philipson’s transition to the biotech sector began with a position at UK-based biotech Trizell, where his efforts culminated in a gene therapy FDA submission for bladder cancer. Four years later at Calliditas Therapeutics, his contributions to drug development in IgA nephropathy led to the FDA approval of Tarpeyo.
XTALKS CLINICAL EDGE: Issue 2 — Calliditas interview
Xtalks Clinical Edge is a magazine for clinical research professionals and all who want to be informed about the latest trends and happenings in clinical trials. This magazine allows you to dive into a world where industry leaders, patient advocates and top researchers converge to bring you the sharpest insights in clinical trials.
IgA Nephropathy
In the US, the prevalence of IgA nephropathy is estimated to range between 130,000 and 150,000 patients, while in Europe, the numbers slightly increase to 150,000 to 200,000 patients.
IgA nephropathy is much more common in China, with estimates of 5 million people with the condition, which could be linked to differences in genetic makeup and environmental factors. Therefore, it is not quite a rare disease there, says Dr. Phillipson.
IgA nephropathy typically manifests in younger adults and for many decades there have not been any effective treatments.
“Many patients have simply had to wait and watch their kidney function decline until eventually they reached end-stage kidney disease and needed to go into dialysis or have a kidney transplant. A huge amount of work has been done to try and understand the condition better,” explains Dr. Philipson.
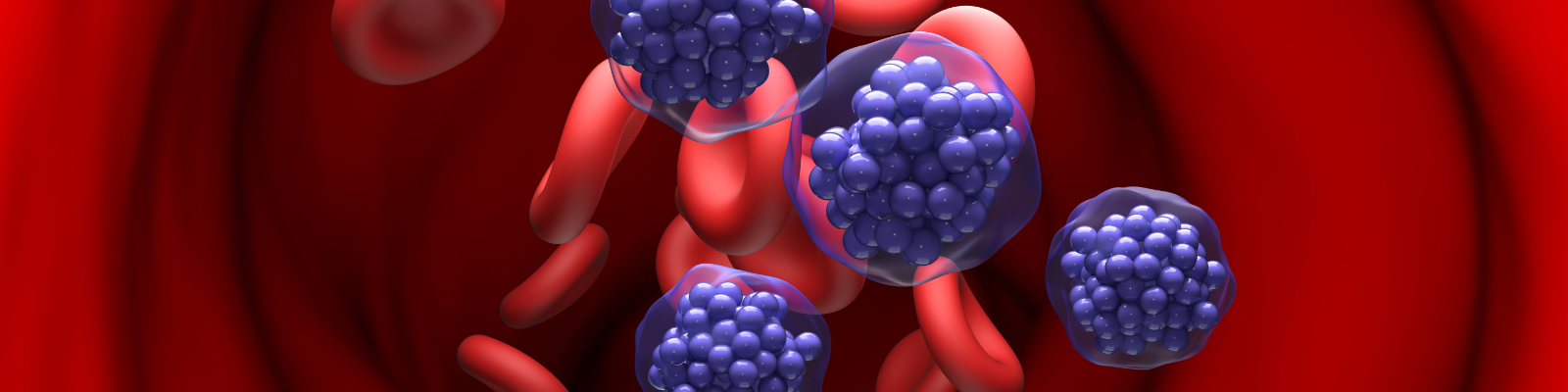
The origins of IgA nephropathy lie in the gastrointestinal tract, specifically in the distal small intestine where there are accumulations of lymphoid tissue called Peyer’s patches, which are mainly made up of B cells and are the source of pathogenic IgA.
Under normal circumstances, IgA should be restricted to the gut as it’s the first line of defense against gastrointestinal infections or other antigenic insults, explains Dr. Philipson.
However, in IgA nephropathy, this pathogenic IgA enters the systemic circulation and due to certain properties of the antibody, elicits an autoimmune response. This leads to the generation of IgG and IgA autoantibodies, which bind to the pathogenic IgA to form immune complexes that circulate and are deposited in the glomeruli (the filtration units of the kidney), eliciting an inflammatory response. This causes the glomeruli to become leaky and over time, inflammation causes damage to the glomeruli, leading to their gradual loss and ensuing decline in kidney function as seen in IgA nephropathy.
TARPEYO® (budesonide) Targeted Release Capsules
Tarpeyo is a unique formulation of the active ingredient budesonide. Tarpeyo has the distinctive property of being readily cleared by the liver (as high as 90 percent of the drug is removed) before it reaches the systemic circulation, which minimizes systemic side effects.
The treatment is designed to target the distal small intestine and due to its formulation, it maintains a sustained high local concentration in the region. It modulates B cells, hampering their ability to secrete pathogenic IgA.
The approval of the drug in the US and Europe represents a milestone in IgA nephropathy treatment.
Cross-Therapeutic Area Learnings and Applications
Calliditas Therapeutics is also developing setanaxib, a NOX enzyme inhibitor for rare diseases as well as cancers.
Setanaxib is a NOX (NADPH oxidase) enzyme inhibitor. NOX enzymes generate reactive oxygen species (ROS), which can accumulate and reach high levels in response to external injuries, causing cellular damage and activation of fibrosis and inflammation pathways.
Calliditas Therapeutics is conducting Phase II clinical trials evaluating setanaxib in primary biliary cholangitis, a rare liver disease, and in a rare lung disease called idiopathic pulmonary fibrosis.
The company also has a Phase II trial looking at setanaxib in patients with head and neck cancer. Results of the trial are expected in the middle of this year.
Dr. Philipson explains that Calliditas Therapeutics is currently exploring partnerships given the potential of setanaxib to treat multiple indications with high unmet needs and the promise of its technology platform.
The drug can target cancer-associated fibroblasts (CAF), which are fibroblasts found in tumors. If there are high levels of CAFs in a tumor, patients tend to respond less well to treatments. The CAFs appear to keep out tumor-infiltrating lymphocytes (TILs), which setanaxib has been shown to reverse in preclinical models. Encouraging TILs into a solid tumor means that checkpoint inhibitors like pembrolizumab work more effectively, as seen in preclinical mouse models.
“I think that could be a really important moment for the field of oncology if we show that with setanaxib, we can change the tumor microenvironment and make treatments like pembrolizumab more effective,” says Dr. Philipson.
Advancing Rare Disease Drug Development Through the Patient Voice
Dr. Philipson recounts that during his decade and a half working in rare diseases, significant advances have been made in the field, particularly with respect to building relationships and including the patient voice.
“We know that rare disease patients have been very poorly served over the years in terms of drug development. I’m really delighted to say that that has changed now.”
The changes owe to an overarching transformation in the field, witnessed through the many different companies, small and large, working in rare diseases, the many treatments now approved for rare diseases, with many more to come, says Dr. Philipson. Although this presents its own challenges such as increased competition, “it’s amazing for patients,” as they have choices now.
One of the most significant aspects in rare disease drug development today is the realization of building effective relationships with doctors, patients and patient organizations.
“You won’t be successful in drug development in rare diseases if you don’t have those kinds of effective relationships,” says Dr. Philipson.
In particular, he says companies and people working in the space have become increasingly aware of the importance of the patient voice in drug development.
This includes involving patients at every stage of drug development. When designing a study, it is critical to think about what it means for a patient, sharing with patients the study plan and receiving their input. For example, it is important to consider the practicality of participating in a clinical trial from a patient’s perspective in terms of the impacts on their daily life.
“If you want to do a study, as we are currently doing in younger patients, like teenagers, what does it mean for them to come into a clinical trial? Can they do it? How does it impact them in terms of the effects on their social life, schooling and family relationships, and what does it mean for their family members to have to support a teenager through a clinical trial?”
These are the kinds of things that may historically, in many areas of drug development, have somewhat been forgotten about and not considered, says Dr. Philipson.
While Dr. Phillipson says the field is getting better on this front, things are not quite there yet.
“We need to continue to develop our skills in that respect and continue to really embrace the patient in the drug development process.”
Reflecting on the evolution of rare disease treatments, Dr. Philipson emphasizes the critical role of understanding disease biology and genetics. “It’s those two things, biology and genetics, that are the linchpins of driving this kind of movement forward,” he explains.
Greater insights into disease biology combined with a concerted effort to build relationships between various stakeholders, from patients to advocacy groups to physicians and clinical study teams, marks a new era of rare disease drug development. As technological advancements progress to help better understand disease biology and design innovative, cutting-edge treatments and clinical studies, the rare disease field is brimming with potential for groundbreaking innovations and breakthrough treatments for patients.
If you want your company to be featured on Xtalks.com, please email [email protected].











Join or login to leave a comment
JOIN LOGIN