Paragonix Technologies, a leading innovator in organ transplant solutions, has performed the first successful pediatric liver transplant using its LIVERguard Donor Liver Preservation System. The procedure was performed by Dr. Deepak Vikraman, a liver transplant surgeon at Duke University Hospital in Durham, North Carolina.
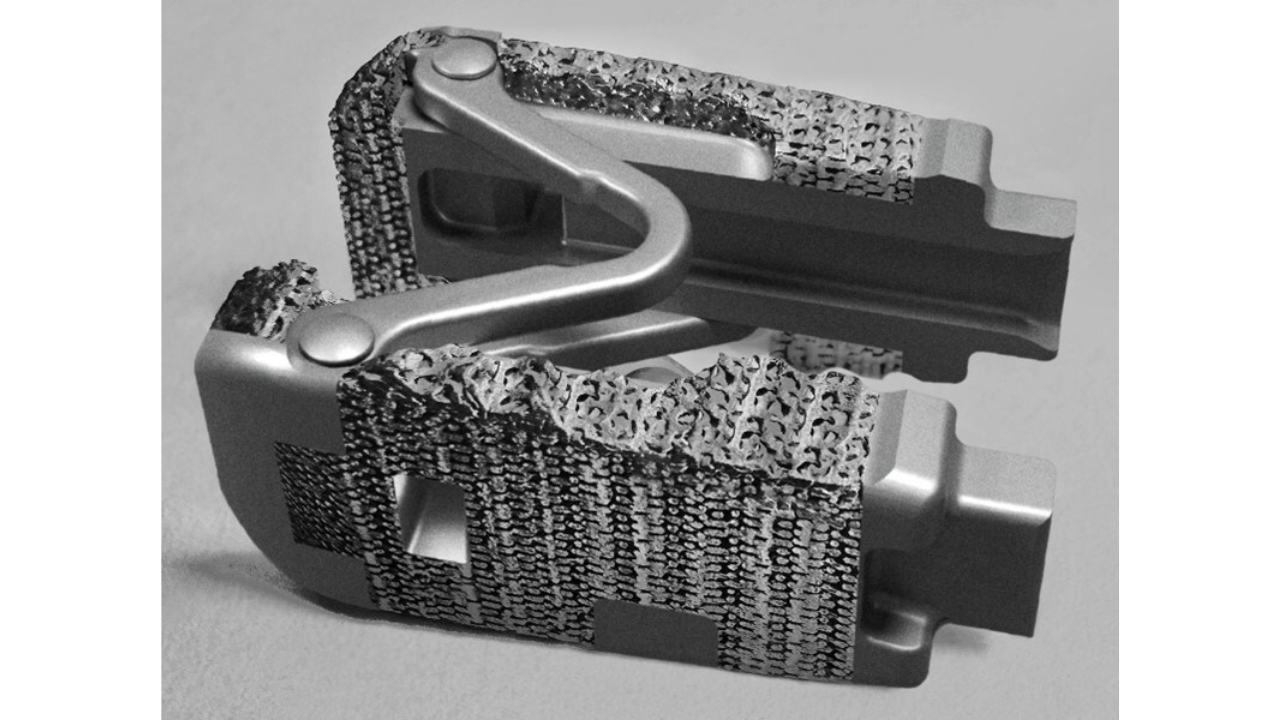
Paragonix Technologies specializes in the development and manufacturing of advanced organ preservation (AOP) devices. Launched in 2021, the LIVERguard system has been employed in over 300 liver transplants across the US, but the recent procedure marks its first application in a pediatric setting.
The LIVERguard System has been shown to reduce post-transplant complications compared to traditional ice storage, as highlighted by recent findings from the GUARDIAN-LIVER global clinical registry. The registry aims to assess the effects of advanced preservation technologies on liver transplantation outcomes.
Related: Lumos Pharma’s Commitment to Innovation in Rare Pediatric Growth Disorders
LIVERguard has significantly enhanced the procurement and allocation of donor livers nationwide, supporting long-distance procurements from locations such as Puerto Rico and Hawaii and enabling organ procurement organizations (OPOs) to utilize high-risk donor livers more effectively.
“This case exemplifies the importance of employing the latest innovations in transplant preservation within pediatric care,” stated Dr. Vikraman in a news release. “By advancing preservation methods, we can expand donor pools and offer young patients a second chance at life.”
LIVERguard offers a highly controlled environment for hypothermic liver preservation, equipped with real-time digital monitoring to safeguard donor organs throughout the transplant process. This represents a substantial improvement over traditional methods that have relied on ice and standard coolers for more than 50 years.
Dr. Lisa Anderson, CEO and President of Paragonix Technologies, expressed enthusiasm for the pediatric application of their system: “We are thrilled to see our technology utilized in the pediatric setting, extending its impact to more liver transplant patients and improving preservation techniques and outcomes for children.”
Challenges and Trends in Liver Transplantation
According to a report published by the US Department of Health and Human Services in 2021, in the US, 36 children died while waiting for a liver transplant or were removed from the list for being too sick. The report found that although living donor transplants offer better outcomes, only 15.4 percent of pediatric liver transplants used living donors, a figure that has not changed significantly over the past decade. The highest pretransplant mortality rate is seen in candidates younger than one year.
However, certain trends in liver transplantation highlight significant shifts in the outcomes for pediatric patients. A recent case at Singapore’s National University Hospital discussed the role of technology in improving pediatric liver transplants. The team successfully used mixed reality imaging to enhance pre-surgical planning for a child with biliary atresia, a rare disease of the bile ducts that manifests in early infancy and requires transplantation in advanced cases.
Another study projected “excellent” survival rates for recent pediatric liver transplants (between 2007 and 2018), with an 88.5 percent patient survival rate at ten years, 84.0 percent at 20 years and 80.1 percent at 30 years. The study concluded that improvements in long-term pediatric liver transplant outcomes are attributable to better surgical techniques, improved management of risk factors and advancements in post-operative care.
These trends underscore the evolving landscape of liver transplantation and the growing demand for innovative technologies to improve surgical outcomes and patient safety.









Join or login to leave a comment
JOIN LOGIN