Clinical trials of certain types of heart disease – including heart failure, coronary artery disease and acute coronary syndrome – are not recruiting enough female patients, according to a study published in the Journal of the American College of Cardiology. Interestingly, the study investigators found that women were often overrepresented in clinical trials of hypertension, atrial fibrillation and pulmonary arterial hypertension.
Despite the sobering statistic that heart disease is the primary cause of premature death among both men and women, diagnostic tools and treatment options are often less effective in female patients. To make matters worse, the lack of women in certain cardiovascular disease trials is having a negative effect on our understanding of which therapies will work well in both genders.
“As we move into the era of precision medicine, that is assessing the impact of a wide range of patient and disease characteristics on drug effects, it is imperative that clinical trial participants represent the full spectrum of patients for whom the drug will be prescribed,” said Dr. Janet Woodcock, senior author of the study and director of the FDA Center for Drug Evaluation and Research. “This will move us closer to our goal of providing the best information possible about the use of drugs for every patient.”
Woodcock and her colleagues looked at the proportion of men and women enrolled in cardiovascular trials over the past decade which were used to support new drug approvals by the FDA. In all, 35 drugs were approved by the regulator between 2005 and 2015 with indications in acute coronary syndrome/myocardial infarction, atrial fibrillation, coronary artery disease including angina, heart failure, hypertension and pulmonary arterial hypertension.
RELATED: Heart & Stroke Launches #TimeToSeeRed Campaign for Women’s Health Awareness
To determine whether the participation of women in these cardiovascular disease trials measured up to the proportion of women in the disease population, the researchers divided the percentage of women involved in trials with the percentage of women affected by the type of heart disease. They established that a number between 0.8 and 1.2 would indicate that women are adequately represented in trials in that disease category. On average, 46 percent of participants in all cardiovascular disease trials studied were female, however this number ranged from 81 percent down to just 22 percent when the gender of participants was studied on a trial-by-trial basis.
While trials of new drugs designed to treat atrial fibrillation, hypertension and pulmonary arterial hypertension were all in, or even above, the 0.8 to 1.4 range for representation of women, this trend was not conserved in all cardiovascular disease trials. Studies of heart failure, coronary artery disease and acute coronary syndrome/myocardial infarction all showed ratios between 0.5 and 0.6, suggesting that women were underrepresented in these studies compared to the incidence of women diagnosed with these heart conditions.
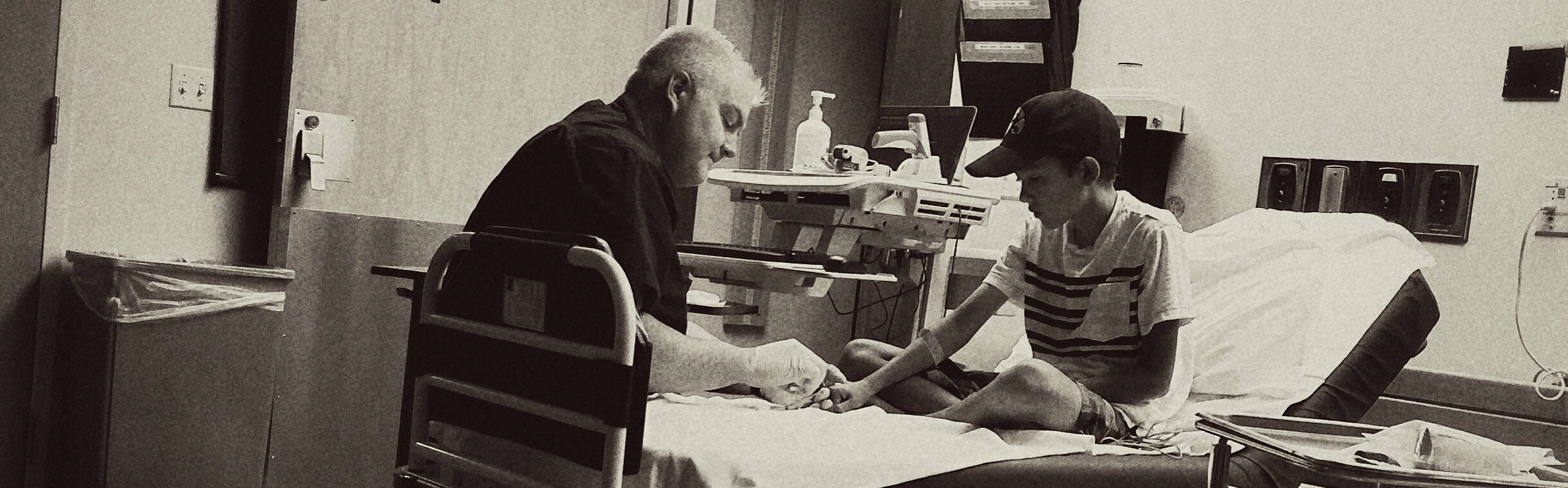
Inclusion and exclusion criteria have previously been found to exclude more women than men from participating in clinical trials of cardiovascular disease, however the researchers identified other factors that they believe could be having an impact on female enrollment. They found that fewer women were being referred for pre-screening – which impacts who can participate in a trial – compared to men. They say that fewer female patients may be identified as potential trial participants, or may not have the ability to participate in a study, which could explain lower enrollment numbers for females.
“Based on this work, future research is needed to identify factors leading to under participation of women in cardiovascular clinical trials, particularly those occurring before screening,” said Dr. Pamela Scott, first author and Director of Research in the FDA Office of Women’s Health. “Research is needed to better define barriers that limit participation of diverse populations, not only of women but of minority and older populations.”
The Heart and Stroke Foundation of Canada recently launched their #TimeToSeeRed campaign aimed at increasing heart disease awareness among Canadian women. This campaign is also designed to propel clinical research into new diagnostics and therapies for heart disease and stroke which may be more effective in women.









Join or login to leave a comment
JOIN LOGIN