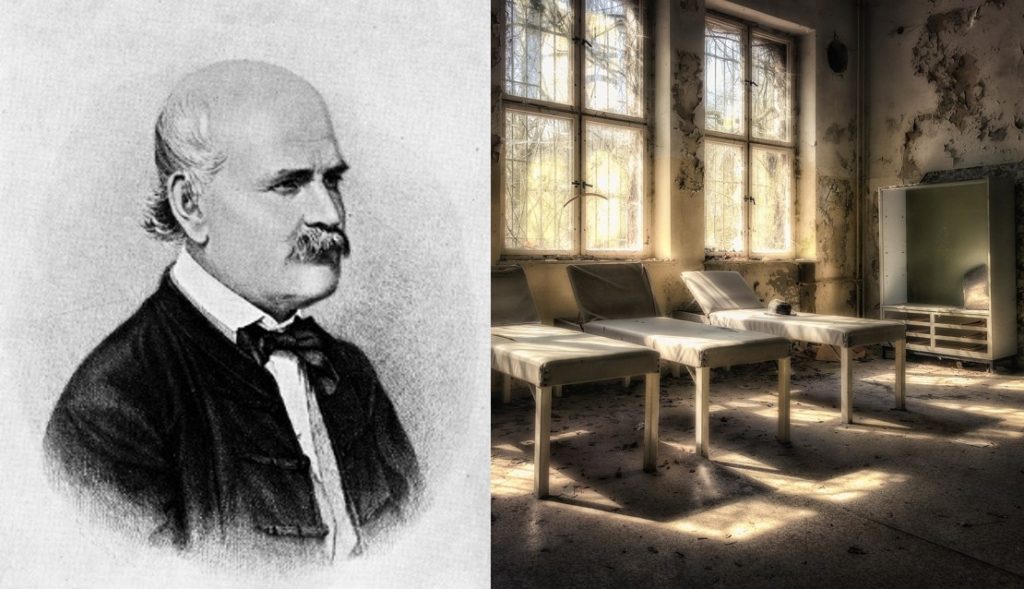
Hand washing is regarded as one of the primary lines of defense against pathogens in our environment. A simple scrub with soap and water can rid our hands of potentially harmful elements including disease-causing bacteria and viruses. While hand washing has been a part of personal hygiene for centuries – as a part of culture, religion and general daily life – its link to disease was only recognized a little over two centuries ago by the Hungarian physician and scientist Ignaz Semmelweis.
Through his work, Semmelweis discovered that maternal deaths during childbirth could be prevented through anti-septic hand washing techniques. As such, he came to be regarded as the ‘savior of mothers’ and an early pioneer of sanitization methods.
Although initially met with resistance by the medical community at the time, Semmelweis’ work laid the foundation for the practice of hand washing by doctors prior to surgery and other medical procedures. Moreover, it led to the universal acceptance of hand hygiene as an important aspect in protecting against pathogen-causing diseases.
Contagion Outbreaks
Disease epidemics and pandemics have been a part of human history since ancient times, particularly as people began to live in more densely populated communities and cities. Infectious disease outbreaks have led to mass quarantines, illnesses and deaths throughout history. Prior to the development of a vaccine for smallpox, the disease was the cause of many epidemic outbreaks, including a significant outbreak in Japan from 735 – 737, which claimed the lives of nearly 2 million people, or a third of the country’s population at the time.
There have been three documented pandemics of the Bubonic plague, which is caused by the bacterium Yersinia pestis. The first pandemic of the plague affected the Eastern Roman, or Byzantine, Empire in the 6th century, which led to 25 – 50 million deaths over two centuries. The third pandemic began in China in 1855 and spread to central Asia and India, where it claimed 10 million lives in the latter country alone.
The Germ Theory of Disease
Up until the later part of the 18th century, there was limited knowledge on the biological causes of the vast majority of human infections and diseases, and importantly, how they were transmitted. It took a long time for ancient medical theories like humorism – in which pathologies were attributed to imbalances of four different bodily fluids, termed ‘humors’ – or miasmas (i.e. ‘bad airs’), to be rejected in favor of evidence-based scientific discovery and knowledge of human health and disease.
It wasn’t until the mid-19th century when the experimental work of Louis Pasteur helped establish the ‘Germ Theory of Disease,’ according to which microorganisms known as pathogens or ‘germs’ give rise to infectious illnesses. The work of scientists like Semmelweis is also largely credited in helping form the basis of the theory.
Pioneering Obstetrics
Ignaz Philipp Semmelweis was born in the Hungarian city of Buda (now a part of the country’s capital Budapest) in 1818 to relatively wealthy merchant parents. His father was of German descent who started out as a grocer and grew his trade to include spices and other consumer goods. Semmelweis was the middle child of ten children.
His foray into medicine occurred after first enrolling in law school at the University of Vienna in 1837; he then switched out after one year to pursue medical school due to unknown reasons. Semmelweis graduated with a medical degree in 1844 and went on to specialize in obstetrics, which was not his first choice of specialty. In 1957, he married Mária Weidenhofer, the daughter of a wealthy merchant who was 19 years his junior, with whom he had five children.
Semmelweis was appointed as an assistant to Professor Johann Klein at the Vienna General Hospital’s First Obstetrical Clinic. The clinic was one of many clinics and institutes set up across Europe to address the growing issue of infanticide of illegitimate children at the time. These maternity institutes provided a place for impoverished and disadvantaged women to seek assistance and be cared for at no fee. In exchange for the free services, the women served as training subjects for doctors and midwives.
Due to the free service, the clinic quickly became overwhelmed with patients, leading to the establishment of a second obstetrics clinic, which was serviced by midwives. The clinics were known as the First Clinic and the Second Clinic.
Childbed Fever
For unknown reasons at the time, it quickly became common knowledge that there was a significantly higher maternal mortality rate at the First Clinic (10 -13 percent) compared to the Second Clinic (2 – 4 percent) due to the development of puerperal fever among the women, which came to be known as ‘childbed fever.’ As a result, the First Clinic had developed a negative reputation, to the point that women would plead to be admitted to the Second Clinic instead of the First.
Some women would even purposely resort to giving birth on the streets on the way to the hospital; this way they could still claim child care benefits without being admitted to the clinic. This practice became widespread enough to be termed ‘street births.’
Semmelweis was perplexed and disturbed by not only the higher mortality rate at the First Clinic, but also by the fact that there was a lower incidence of illness even in women who gave birth out on the street.
He noted (in a book he published) that “To me, it appeared logical that patients who experienced street births would become ill at least as frequently as those who delivered in the clinic…What protected those who delivered outside the clinic from these destructive unknown endemic influences?”
He decided to pursue investigation into the matter and began by first asking the First Clinic to switch or change procedures. Among these was the position in which women gave birth: in the Second Clinic staffed by midwives, women gave birth laying on their side whereas in the First Clinic, women gave birth on their back. It was found that changing birthing position did not make any difference to mortality rates. He even went so far as incorporating religious aspects into his queries, removing priests who would walk through the First Clinic with bells, hypothesizing that the loud clamouring may be terrorizing the women. Once again, none of these approaches led to any changes in the childbed fever-related mortality rate at the clinic.
Semmelweis’ experimentations thus far did not yield any tangible results, except for Semmelweis’ demotion by unimpressed and annoyed hospital administration as his work was not received well at the hospital. Hospital colleagues and officials thought he was stubborn and arrogant and as such, were unwilling to cooperate with him.
Despite the pushback and resistance at the hospital, Semmelweis remained steadfast in his pursuit of answers.
Breakthrough
Frustrated, Semmelweis went on a one-month long vacation in the Austrian countryside. This may have been a much-needed break as when he returned, he began to notice pertinent details in the routines and practices of doctors at the maternity clinic.
His breakthrough finally came in 1947, through an unfortunate accident that caused the death of his friend and colleague Jakob Kolletschka, a professor of forensic medicine at the Vienna hospital. Kolletschka was training a student during which he injured his finger with a scalpel while performing an autosopy, leading to infection and death within days.
Upon reviewing Kolletschka’s autopsy records, Semmelweis found that his friend had suffered the same symptoms of puerperal fever as the women in the maternity clinic. Moreover, he realized doctors were performing autopsies on cadavers in the morning prior to seeing patients in the maternity First Clinic. This almost immediately led Semmelweis to hypothesize that contaminants from cadavers remaining on the hands of doctors may be the cause of the puerperal fevers.
To test this, he asked doctors to wash their hands with chlorinated lime, or calcium hypochlorite (much like household bleach), to get rid of ‘cadaverous particles’ before birthing patients. The doctors took great offense to this, appalled that they were being accused of transferring pathogenic material to their patients, and disgruntled at having to wash their hands with a harsh substance.
Nevertheless, Semmelweis’ experiment led to positive results as he found that mortality rates from puerperal fever in the maternity clinic dropped by a dramatic 90 percent after implementation of the stringent hand washing procedure. In fact, within just a few months, mortality had reached zero percent.
Skepticism and Rejection from the Medical Community
Although Semmelweis’ results were clear, he could not provide a scientific basis for his observations, which led to widespread skepticism of his theory. The medical community therefore remained unconvinced, which along with the displeasure of colleagues and staff at the institution, led to his dismissal from the Vienna hospital. After his departure, hand washing was abandoned, leading mortality rates to rise steeply.
After being ousted from Vienna, he obtained an appointment at a hospital in Budapest. He was not welcomed by the medical community there either for his seemingly outrageous thoughts and claims on hand washing and cleanliness in fighting infection. Nevertheless, Semmelweis continued his advocacy for hand washing, reportedly stopping young couples in the streets, begging them to ask their doctors to wash their hands before delivering any future child that they may have.
Semmelweis grew increasingly frustrated and emotionally and mentally unstable from being antagonized and shunned by colleagues and the general medical community, who were still latched onto humoral and miasmatic schools of thought.
While he refused to formally publish his scientific findings, Semmelweis eventually ended up writing a book (The Etiology, Concept and Prophylaxis of Childbed Fever) in which he outlined his observations of reducing childbed fever-related mortality through hand washing, while lambasting those that rejected and opposed his ideas, calling them ‘murderers.’
Tragic End
Semmelweis began having nervous breakdowns and suffered from bouts of severe depression. He became fixated on hand washing and childbed fevers, driving every conversation to the topic. As he became increasingly unstable, he was deceived into being admitted into a mental institution.
His life came to an ironic and tragic end in 1865 at the age of 47 after he was beaten by guards at the asylum after a reported escape attempt. As a result, he developed a gangrenous infection in his hand, which led to his death just 14 days later due to septicemia (septic shock), the very disease that he had fought tirelessly against and helped saved many women from through his discovery of hygiene-based hand washing.
Championship and Legacy
Semmelweis unfortunately did not live to learn about Pasteur’s Germ Theory work, through which he proved just a few years later that bacteria were the contagions underlying infectious diseases, including puerperal fevers.
Pasteur’s work led the Scottish surgeon Joseph Lister to test the use of carbolic acid as an anti-septic on wounds and surgical tools, along with washing his hands, before performing surgery. The results of the approach were positive, and although met with initial skepticism, the widespread implementation of scrubbing hands and sterilization of surgical tools in surgery was in place by 1875.
Semmelweis’ legacy is profound as he is credited as a significant contributor to Germ Theory through his tireless efforts linking hand germs to infectious disease. He is championed as the father of hand hygiene and a pioneer of infection control.








Join or login to leave a comment
JOIN LOGIN