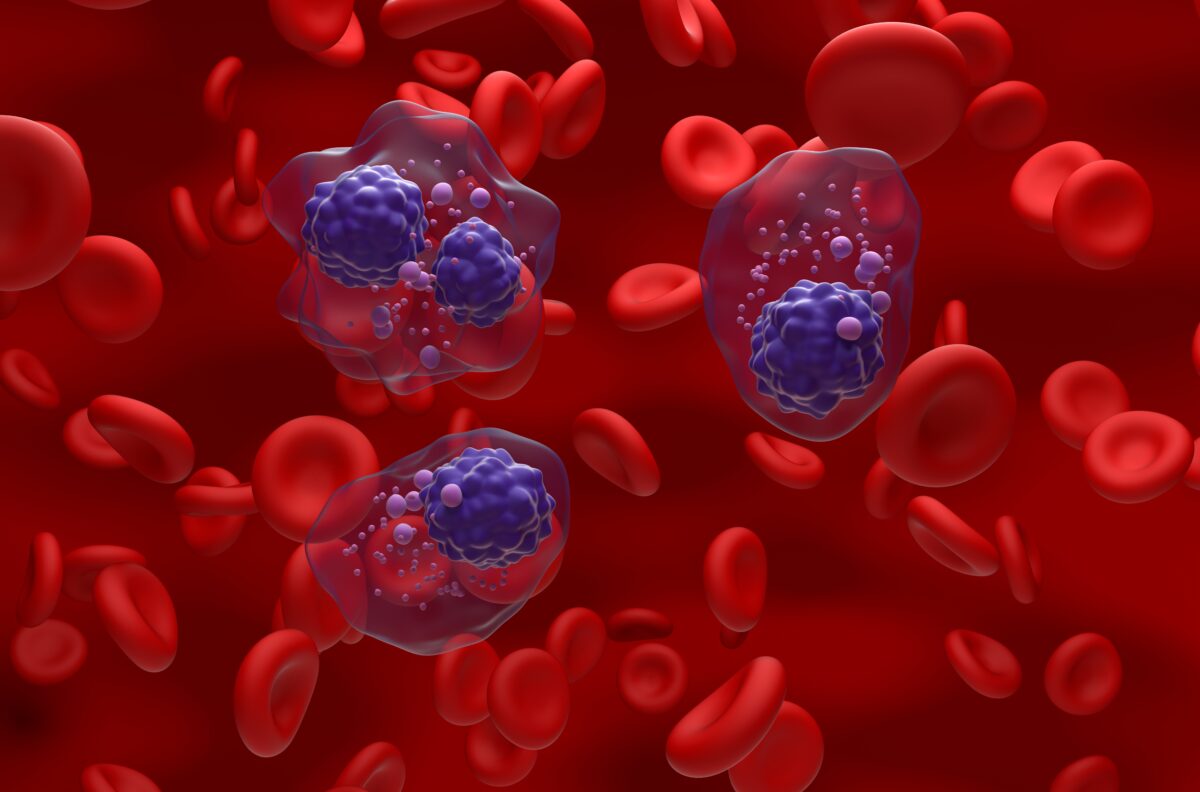
The induction phase of chemotherapy treatment can have a dampening effect on pediatric acute lymphoblastic leukemia (ALL) patients’ immune systems, leading them open to life-threatening infections. Now, researchers at St. Jude Children’s Research Hospital have found an antibiotic that could help prevent patients from contracting these infections, without contributing to antibiotic resistance.
When a patient is first exposed to chemotherapy, they often experience neutropenia, in which their white blood cell count drops and their ability to fight infection becomes compromised. Subsequent infections can delay treatment timelines, and in up to 4 percent of cases, can be fatal.
“This research provides the first major evidence supporting targeted use of antibacterial prophylaxis for at-risk pediatric ALL patients, particularly use of the broad-spectrum antibiotic levofloxacin,” said Dr. Joshua Wolf, an assistant member of the St. Jude Department of Infectious Diseases.
The study was the largest of its kind to investigate whether providing antibiotics along with chemotherapy treatment in pediatric ALL patients would be both safe and effective at minimizing the risk of infection. Wolf and his colleagues published their findings in the journal, Clinical Infectious Diseases.
The researchers found that prophylactically treating ALL patients with the antibiotic drug levofloxacin, reduced the risk of infection by 70 percent during the induction phase of chemotherapy. The drug also reduced the odds that patients would contract hospital-acquired Clostridium difficile infection, which is associated with a higher rate of mortality.
Further, the proactive antibiotic treatment reduced the need for patients to be treated with common antibiotics, such as vancomycin and cefepime, which are often prescribed when a patient develops an infection during cancer treatment. According to Wolf, these results could support the routine use of levofloxacin in pediatric patients with ALL.
“Prophylactic antibiotic therapy with levofloxacin is routine for at-risk adult ALL patients, but it has remained controversial in children,” Wolf said. “Until this study, evidence supporting the safety and efficacy of prophylactic antibiotic therapy in children with ALL has been sparse.”
In all, 344 patients were included in the study, as part of the St. Jude Total XVI clinical trial for newly-diagnosed ALL patients. The hospital now recommends that ALL patients who develop neutropenia during the induction phase of chemotherapy be prophylactically treated with levofloxacin, provided their condition is expected to last for a week or more.
“We are cautiously optimistic that any impact of levofloxacin on antibacterial resistance will be balanced by the reduction in use of other antibiotics, but long-term monitoring of antibiotic resistance patterns in young ALL patients will be needed to prove this,” said Wolf.











Join or login to leave a comment
JOIN LOGIN