The prostate-specific antigen (PSA) test for prostate cancer screening has long been criticized for overdiagnosis and overtreatment, while having little effect on reducing prostate cancer mortality. Currently, there are no unanimous screening recommendations using the PSA test, creating discrepancies over how prostate cancer patients are cared for around the world.
Biotech company Cleveland Diagnostics hopes their revamped PSA test will improve the outlook for men in the US, where 192,443 new cases of prostate cancer were reported in 2016. Last week, the company received US Food and Drug Administration (FDA) Breakthrough Device Designation for their test, IsoPSA.
“We are very grateful that [the] FDA recognizes the potential of IsoPSA, the first test in our pipeline of simple, affordable, and highly accurate cancer tests that focus on cancer-relevant changes to protein biomarkers in blood,” said Dr. Arnon Chait, CEO of Cleveland Diagnostics, in a statement. “We look forward to working closely with [the] FDA to expedite the appropriate approvals and get this important new test into the hands of physicians.”
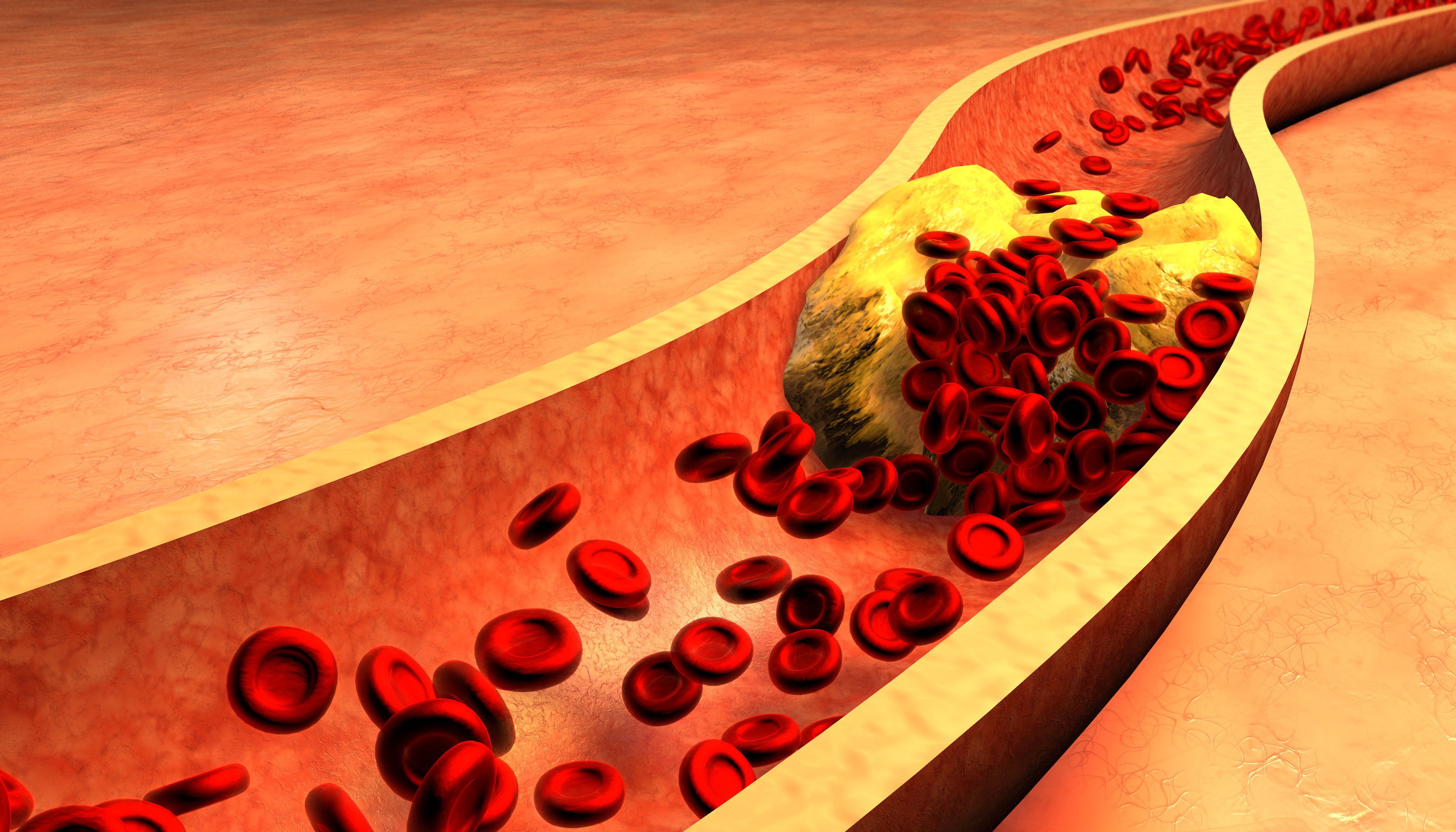
What makes IsoPSA different from traditional PSA tests? It measures PSA protein that’s undergone structural changes due to cancer mutations rather than overall PSA levels. The blood sample is added to a biphasic system comprising two immiscible solvents that separate out proteins based on their structure and interaction with other proteins.
This type of analysis is different from a traditional PSA test. Traditional tests measure total PSA protein in the blood, which can be released by normal cells and cancer cells, plus levels can fluctuate due to inflammation, infection, medication and old age. Therefore, elevated levels of PSA protein may not actually signal prostate cancer, but a physician may recommend additional invasive tests such as digital rectal examination or prostate biopsy. These procedures are not only expensive, but they may pose serious health risks.
In light of these issues, the American Urological Association guidelines recommend against PSA screening in men under age 40 and routine interval screening every two years should reduce overdiagnosis and false positives.
According to a validation study, the Cleveland Diagnostics test had greater specificity compared to the traditional PSA test, meaning it is superior at correctly identifying individuals without prostate cancer. Still, the test is only fit for initial screening; further diagnostic tests will need to be conducted.
While Cleveland Diagnostics is set on another blood-based biomarker test, other companies have opted for urine tests and even breath tests. Multiparametric magnetic resonance imaging (MRI) gives clinicians a comprehensive view of the prostate so they can take biopsies as needed.
Prostate cancer remains a leading cause of cancer in men, killing 30,370 US males in 2016. Early detection and diagnosis can help patients get faster access to treatments and improve their prognosis down the road.
“Clinicians today are using an array of diagnostic tests and procedures to inform decisions about a patient’s prostate health and the risk of prostate cancer,” said Dr. Mark Stovsky, urologist and CMO of Cleveland Diagnostics. “We believe that IsoPSA has the potential to fill a major void in this space.”
The company plans to commercialize IsoPSA in the US by next year.









Join or login to leave a comment
JOIN LOGIN