Using human pluripotent stem cells, researchers at Cincinnati Children’s Hospital Medical Center have developed colon-like organoids that can be transplanted into mice. The study – published in the journal, Cell Stem Cell – could provide researchers with a better model of human gastrointestinal diseases.
According to the researchers, this could be the first tune that tissue mimicking the structure and function of the human colon has been made. Along with the ability to study diseases of the gastrointestinal (GI) tract – including Crohn’s and other forms of irritable bowel syndrome (IBS) – the tissue engineering technique could eventually be used to generate organoids for transplantation into human patients.
“Diseases affecting this region of the GI tract are quite prevalent and include ailments like colitis, colon cancer, irritable bowel syndrome, Hirschsprung’s disease and polyposis syndromes,” said senior study author Dr. James Wells, director of the Cincinnati Children’s Pluripotent Stem Cell Center. “We’ve been limited in how we can study these diseases, including the fact that animal models like mice don’t precisely recreate human disease processes in the gastrointestinal tract. This system allows us to very effectively model human diseases and human development.”
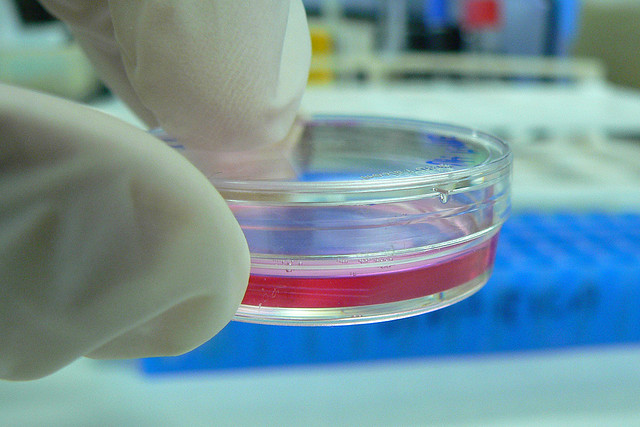
Wells and his team have been growing organoids using human pluripotent stem cells (hPSCs) in their lab since 2009. They have successfully grown embryonic small intestines and certain regions of the human stomach, however the researchers say that the colon proved challenging to build in vitro.
Part of the problem was a lack of available information about how the colon develops in humans during embryogenesis. Using a number of molecular and genetic screens, the researchers were able to identify important markers for early development of the organ.
To test the lab-grown organs, the researchers transplanted the tissue into the tough layer that surrounds the kidney – known as the kidney capsule – of immunosuppressed mice. Over a 10-week period, Wells and his colleagues monitored the mice for signs of the hormone-secreting posterior region enteroendocrine cells found in the fully-developed human colon.
They found that the transplanted colonic organoids showed molecular, cellular and structural characteristics of the human colon. This type of organoid could also help drugmakers conduct preclinical studies of new therapeutic compounds.
“By exposing human colonic organoids to inflammatory triggers, we can now learn how the cell lining of the colon and the supporting cells beneath cooperate to respond to inflammation,” said primary author Dr. Jorge Munera, postdoctoral fellow in the Wells laboratory. “This could be very relevant for patients with Crohn’s disease or ulcerative colitis. And because the microbiome, the organisms that live in our guts, are most concentrated in the colon, the organoids potentially could be used to model the human microbiome in health and disease.”











Join or login to leave a comment
JOIN LOGIN