As reported by Statista, in 2021, the US allocated 17.8 percent of its gross domestic product (GDP) to healthcare, amounting to a whopping 4.4 trillion US dollars in 2022.
The burden of chronic diseases and obesity is particularly severe in the US; the 2020 Commonwealth Fund International Health Policy Survey revealed that 30.4 percent of adults reported having two or more chronic conditions such as heart disease, diabetes and depression. A study on the social determinants of health in the US reported that Black infants had a higher mortality than White infants (11.4 vs. 4.9 per 1000 live births).
The US continues to experience the highest amenable mortality rate, which is the rate of premature deaths from chronic conditions that could be prevented by timely and quality care.
Additionally, a notable 43 percent of respondents, aged 16 to 74, expressed complete dissatisfaction with the US’s national healthcare system.
All of this is to say that despite the US spending a significant portion of its GDP on healthcare — more than any other high-income country — the health outcomes do not match this investment. The only country to not have universal healthcare, the US suffers from poorer health outcomes, including lower life expectancy, high hospitalization rates and higher rates of preventable deaths.
The National Institutes of Health (NIH) aims to address this crucial gap, improving the efficiency and effectiveness of healthcare delivery with evidence-based primary care models that focus on prevention and early intervention.
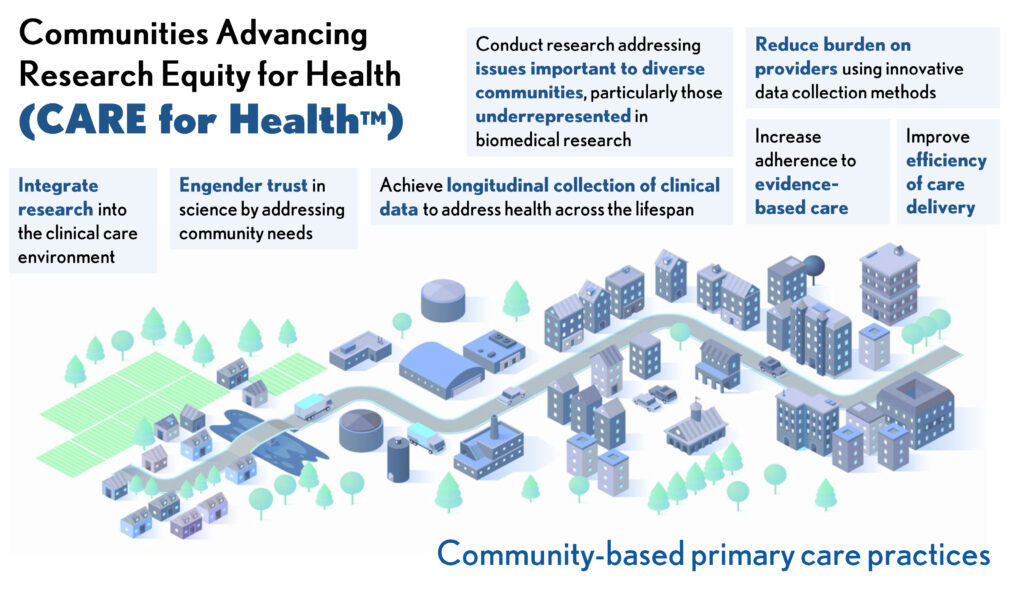
The NIH is pioneering a new initiative called the “Communities Advancing Research Equity for Health” (CARE for Health). With an investment totaling $30 million across fiscal years 2024 and 2025, this program seeks to enhance patient care, particularly in communities that have historically been underrepresented in clinical research or underserved by healthcare systems.
CARE for Health will integrate clinical research with community-based primary care. The initiative plans to grow an evidence base that will support both underserved populations and clinicians by informing medical care, improving patients’ understanding of clinical trials and opportunities to participate in them and providing access to the best scientific research.
XTALKS WEBINAR: Bridging the Gaps: Diversity, Retention, and the Role of Optimized Trials in Modern Clinical Research
Live and On-Demand: Tuesday, July 23, 2024, at 1pm EDT (10am PDT)
Register for this webinar today to explore the transformative potential of decentralized clinical trials and how optimized and virtual-first trials are addressing longstanding challenges in clinical research.
Community-Based Primary Care Centered on Diversity and Inclusion
The CARE for Health program aims to establish a national primary care research network that not only expands access to clinical research but also tailors it to the specific needs of diverse communities.
The willingness of underrepresented groups to participate in research is often underestimated. Studies indicate that if asked, individuals from diverse racial and ethnic backgrounds show a similar or even greater willingness to engage in clinical research compared to other groups.
However, systemic barriers, such as lack of access to healthcare, transportation issues and structural barriers within the research infrastructure, often prevent their participation. A study conducted with 17 Black women at high risk for HIV found that despite their favorable attitudes towards medical research, historical distrust in the medical treatment offered to Black Americans became a deterrent towards participation in HIV vaccine trials.
Several Black Americans also mentioned the Tuskegee syphilis study when declining participation or expressing unwillingness to participate in clinical trials. Other studies have also underscored the facilitators to patient enrollment in clinical trials, including culturally and linguistically competent research teams, the inclusion of family members in the dialogue on patient participation, compassionate and personalized interviews and more.
NIH Director Dr. Monica M. Bertagnolli, emphasized the importance of adapting research to be inclusive, citing the deteriorating health outcomes in significant US population segments despite scientific advancements.
Dr. Bertagnolli highlighted that community-based primary care engendered trust and confidence in recommended medical care or science. “In fact, greater availability of primary care services in communities is associated with fewer disparities in health outcomes and lower mortality. We earn people’s trust when they get access to the care they need and when they can see direct benefits from their participation in research,” she added in the press release.
Ensuring Health Equity by Expanding Access and Reducing Disparities
CARE for Health’s community-driven approach is expected to yield the best outcomes by ensuring that all communities have equal access to the newest and most effective treatments and health strategies.
As CARE for Health expands, it will launch new studies, establish additional study sites and enhance data management and interoperability to facilitate a learning health system where clinical practice and research inform each other. The goal of a learning system is to provide better patient outcomes and more favorable environments for healthcare providers. This is driven by the need to shift from volume-based care to value-based care.
Moreover, breaking down the traditional silos between medical care and community services to prevent diseases before they occur is a critical component of this model, rewarding providers and health systems based on results rather than mere activities.
The initiative will use the NIH Common Fund to initially collaborate with existing NIH-funded clinical research networks and community partners to build the necessary infrastructure at select primary care sites. The first round of funding, expected in the fall of 2024, will target organizations that primarily serve rural areas, aiming to bring advanced research opportunities to regions often overlooked in health innovation.
“Health is dependent upon many factors. We recognize that environmental and societal factors are very important, and that each community is unique. Because of this, we must adapt our research to be more inclusive and more responsive to the needs of communities currently underserved in health research,” stated Dr. Bertagnolli in her vision for the program.
The NIH had also scheduled a public workshop to discuss the integration of research into primary care, aiming to gather input on overcoming challenges and seizing opportunities in this transformative approach to healthcare.
Enhancing Patient Engagement through Direct Involvement
For patients, the CARE for Health initiative means more direct involvement in the research that shapes their healthcare. Participating sites will choose research studies based on local health priorities, allowing patients to contribute data and receive research findings that are relevant and beneficial to the community’s health needs. This approach will empower patients and enhance trust in the healthcare system by demonstrating tangible benefits from research participation.
CARE for Health is designed to allow primary care providers and their patients to actively contribute to and benefit from the generation of medical knowledge. This integration aims to improve patient outcomes by making the latest research directly applicable to everyday medical care.
The program will focus on demographic groups that are often overlooked in healthcare provisions and medical studies, such as racial and ethnic minorities, older adults, residents of rural areas and individuals with low socioeconomic status or lower educational attainment.
The community-based primary care initiative represents a significant step towards realizing a healthcare system that is as diverse and inclusive as the population it serves. Health and Human Services (HHS) secretary Xavier Becerra said on the broader impact of the program, “Health research should be accessible to all populations. Clinical trials should reflect the diversity of Americans — because we know that delivers the best results.”











Join or login to leave a comment
JOIN LOGIN