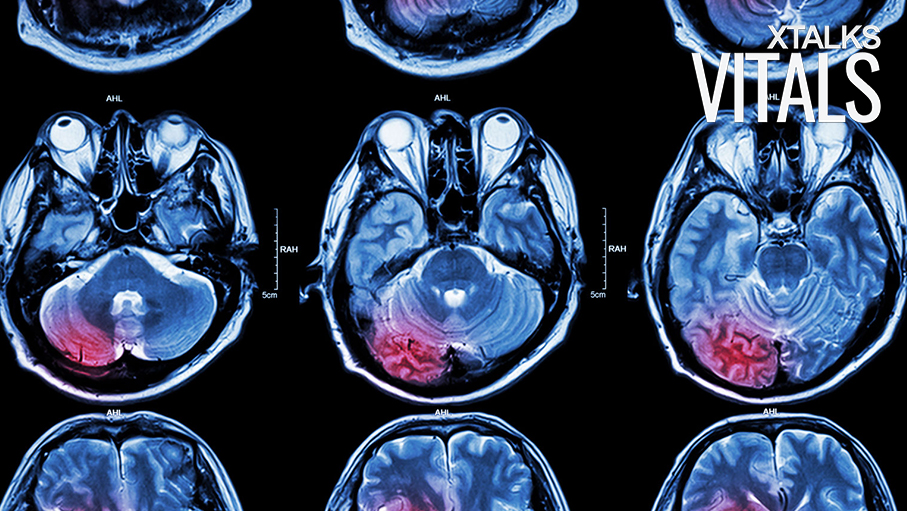
A Phase I clinical trial testing whether CAR-T cell immunotherapy could be a viable treatment for a type of brain cancer known as glioblastoma, has found that the therapy was both safe and effective. The researchers used T cells collected from each participant, and engineered them to target a specific protein – known as EGFRvIII – which is expressed in approximately 30 percent of glioblastomas.
The researchers chose to target the EGFRvIII protein because it’s only found in tumor tissue. By choosing a protein that’s not expressed in heathy cells, the researchers hope the therapy may have fewer side effects compared to other CAR-T cell treatments.
While the immunotherapy has only been tested in nine patients so far, the safety profile was acceptable across all participants. No patients showed signs of a potentially serious immune reaction – known as systemic cytokine release syndrome – which has been a safety issue in other CAR-T trials. While one patient experienced a seizure after receiving the CAR-T cell infusion, the patient was successfully treated with antiepileptic medications.
The study investigators found that between seven and ten days post-infusion, all patients displayed significant expansion of the CART-EGFRvIII cells in their blood. When tumors were surgically removed from five of the patients between days six and 120 after the infusion, focal areas showed that both CAR-positive and CAR-negative T cells were able to infiltrate the cancerous tissue.
“One of the main questions in the field of T cell therapies is: can we make this work in solid tumors?” said Dr. Marcela Maus, Director of Cellular Immunotherapy at the Massachusetts General Hospital Cancer Center, and a Member of the Faculty at Harvard Medical School.* “The barriers to CAR-T cells in solid tumors are identifying targets with acceptable safety profiles, proving that T cells can get out of the blood, and that they can successfully target the tumor cells expressing the antigen without being turned off by the tumor environment.”
“Here, we demonstrated that targeting EGFRvIII has an acceptable safety profile, , that CAR-T cells do actually find their way and get into the tumor – even crossing the blood-brain barrier – and are able to eliminate the target,” said Maus. Maus worked alongside Dr. Donald M. O’Rourke, an associate professor of Neurosurgery at the Perelman School of Medicine at the University of Pennsylvania.
Glioblastomas affect over 22,000 Americans each year. Patients with glioblastomas that are EGFRvIII-expressing tumors tend to respond poorly to standard tumor therapies.
“We now need to see in the next set of patients if we can augment the effects of the CAR infiltration into the brain and determine optimal timing and combination of this therapy with other established therapies,” said O’Rourke. “In this manner, we believe this highly personalized T cell therapy will begin to show clinical efficacy in a reproducible manner with all patients containing EGFRvIII-positive GBMs.”
*Editor’s Note: Dr. Marcela Maus’ job title was changed to reflect her position at Harvard Medical School.









Join or login to leave a comment
JOIN LOGIN