The pioneering CRISPR gene editing technique has just received a serious upgrade; researchers at the University of California, San Francisco, have developed an electroporation technique capable of introducing the CRISPR enzymes into cells without the need for a viral vector. The team – who published their findings in the journal Nature – were able to use this modified CRISPR technique to successfully edit the DNA of human T cells.
According to the researchers, this technique is fast, versatile and economical enough to be widely adopted by those developing new therapies to be used to treat conditions like cancer, autoimmune diseases and inherited genetic disorders and defects. Since the creation and availability of viral vectors have represented a significant hurdle for those developing cell and gene therapies, the researchers believe that a virus-free approach could accelerate the development of new CRISPR-based therapies. In addition, the current technique could a be a more targeted way to edit the genome as viral vectors can introduce genes into off-target areas of the genome.
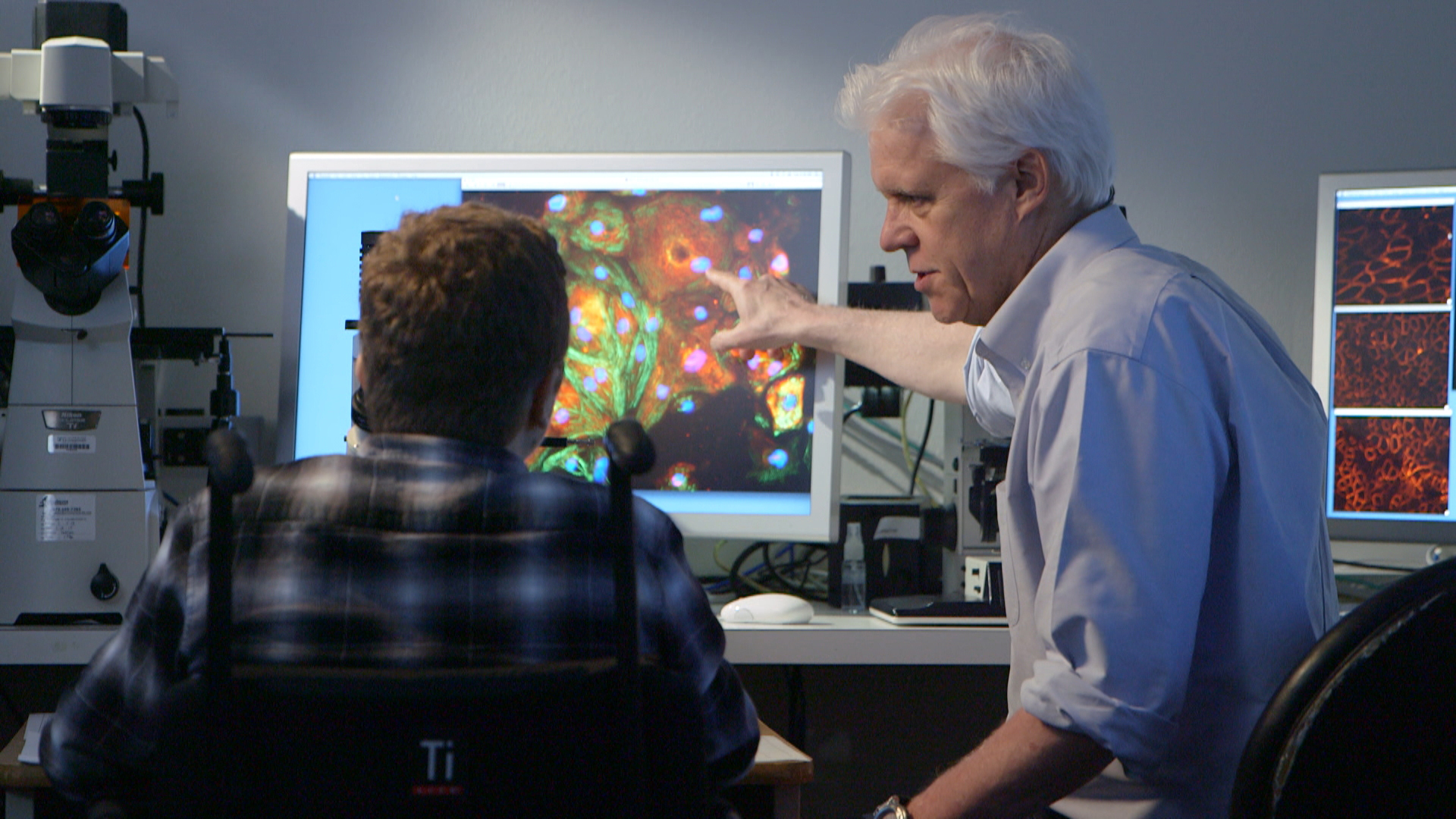
“This is a rapid, flexible method that can be used to alter, enhance, and reprogram T cells so we can give them the specificity we want to destroy cancer, recognize infections, or tamp down the excessive immune response seen in autoimmune disease,” said UCSF’s Dr. Alex Marson, associate professor of microbiology and immunology, and senior author of the new study. “Now we’re off to the races on all these fronts.”
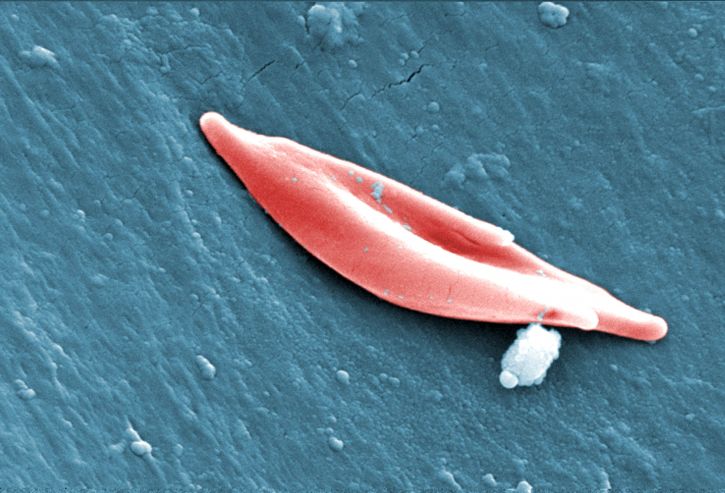
As a viral vector is normally required to get the CRISPR components into the cells to be edited, Marson and his team sought to find an alternate route. After optimizing the amount of CRISPR enzymes and DNA designed to edit a set number of T cells in a sample, the researchers exposed the cells to an electrical field in a process known as electroporation. This electrical field temporarily makes the cell membrane more permeable, allowing the CRISPR components to enter the cell. From there, they’re localized to the nucleus where they were successful at cutting specific spots in the genome and integrating newly-introduced sequences into the DNA.
The current study is also the first to demonstrate that long stretches of DNA can be integrated into the genome using this CRISPR technique. Previous work found that only short snippets of code could be introduced in order to avoid killing the cells altogether.
The researchers tested their altered CRISPR technique in two unique experiments which serve to highlight its versatility. Marson and his team demonstrated that the technique could reverse the IL2RA mutation in T cells which causes a rare autoimmune condition in children. In another experiment, they used the same CRISPR technology to engineer T cells to target and destroy melanoma cancer cells.
“There have been thirty years of work trying to get new genes into T cells,” said first author Theo Roth, a student pursuing MD and PhD degrees in UCSF’s Medical Scientist Training Program who designed and led the new study in Marson’s lab. “Now there should no longer be a need to have six or seven people in a lab working with viruses just to engineer T cells, and if we begin to see hundreds of labs engineering these cells instead of just a few, and working with increasingly more complex DNA sequences, we’ll be trying so many more possibilities that it will significantly speed up the development of future generations of cell therapy.”
According to Roth, the technique has already revolutionized the way they do research in their lab. Because custom T cells can be produced using this updated version of CRISPR in little more than a week, the team is able to start new projects that would have otherwise been prohibitively expensive or too difficult to pursue.
“We’ll work on 20 ‘crazy’ ideas,” Roth said, “because we can create CRISPR templates very rapidly, and as soon as we have a template we can get it into T cells and grow them up quickly.”






Join or login to leave a comment
JOIN LOGIN