Now a common gene editing tool, the popularity of the CRISPR-Cas9 system has increased over the past decade. CRISPR is notable for engineering living cells, allowing scientists to edit, turn off, delete, or replace genes in a cell’s genome. This technology has powerful implications for therapeutic uses, such as replacing mutated or disease-causing genes or increasing the activity of cancer-fighting cells.
Viral vectors have traditionally been used in gene editing where the shells of viruses carry the template DNA into cells, but this method has its disadvantages. It is difficult to control where the viral vectors insert genes in the genome, and it is difficult to manufacture large quantities of clinical-grade viral vectors.
CRISPR technology has begun to enter clinical trials due to emerging therapeutic applications, but the technology still has limitations, primarily because it is difficult to safely make large quantities of precisely edited cells. However, researchers are determined to overcome this hurdle.
In a press release last week, it was announced that novel CRISPR research completed by a group at the Gladstone Institutes and UC San Francisco had been published in Nature Biotechnology. The goal of the team was to significantly increase yields of correctly engineered immune cells with CRISPR to effectively manufacture cell therapies.
Alex Marson, MD, PhD, and senior author of the study states that the research team has developed a method to insert lengthy DNA sequences into a target site in the genome without the use of viral vectors. The results demonstrate potential as a novel, safe and effective approach to cell therapies.
Harnessing the Cellular Engineering Potential of CRISPR
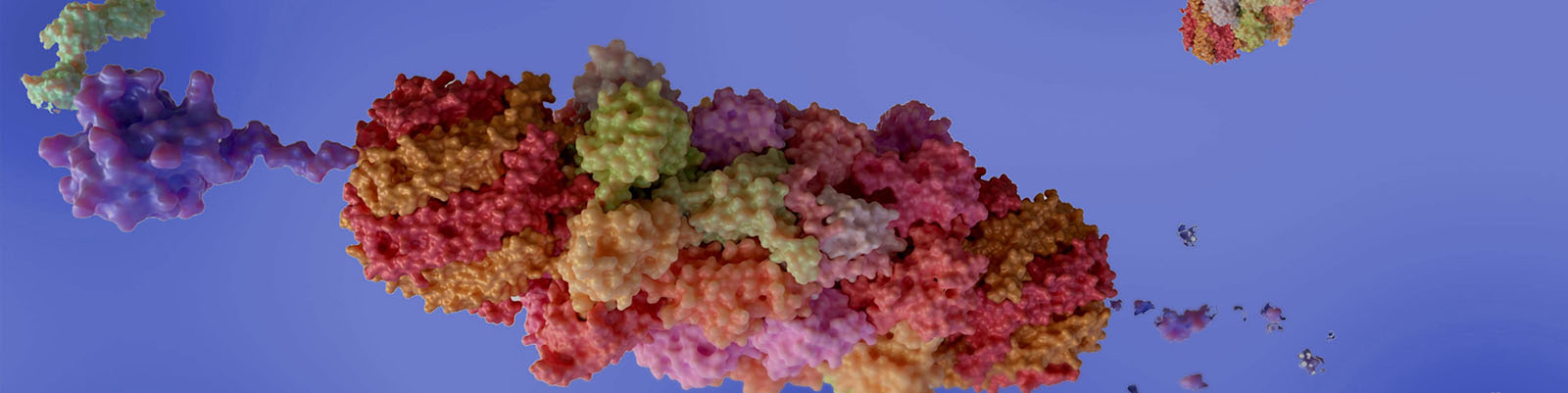
The CRISPR-Cas9 system works by having “spacer” sequences transcribed into short RNA sequences that can guide the system to the matching target in the DNA sequence of a cell. Once the target DNA is found, the Cas9 enzyme binds to the DNA and cuts it, which can turn the gene “off” or allow for the insertion of specific DNA sequences. In cells, DNA exists as both single and double strands, and Cas9 specifically attaches to double-stranded DNA.
Marson’s group initially collaborated with CRISPR pioneer Jennifer Doudna, PhD, in 2015. During this time, they successfully inserted short DNA templates into cells without the use of viral vectors by using an electrical field to make the cell outer membrane more permeable. By 2018, they were able to insert longer DNA sequences into cells with CRISPR, and in 2019 they found that using a modified version of the DNA templates that bind to the Cas9 enzyme (which cuts the cellular genome during CRISPR gene editing), they could efficiently insert DNA sequences into the target site.
Over the course of the study, they observed that large quantities of double-stranded DNA templates were toxic to cells, so their approach could only be used with small amounts of the template DNA and resulted in lower efficiency.
On the other hand, single-stranded DNA is less toxic to cells even in large quantities, so they developed a method to attach a modified Cas9 enzyme to a single-stranded DNA template by adding a short overhang of double-stranded DNA at the end of the template. With the advantages of both approaches combined, the single-stranded DNA substantially increased the efficiency of gene editing, while the double-stranded ends of the templates allowed the team to use Cas9 to improve the delivery of the template DNA into the cells.
Using this novel technique, the team also demonstrated that they could generate over a billion CAR-T cells, which are T-cells that have been genetically modified to fight the cancer cells that cause multiple myeloma. In their experiments, half of the T-cells gained the gene that converted them to CAR-T cells due to specific targeting of the TRAC site in the cells’ genome.
From the Bench to Patient Therapeutics
“We showed that we can engineer more than one billion cells in a single run, which is well above the number of cells we need to treat an individual patient,” states Brian Shy, MD, PhD, and first author of the study.
The team’s approach to cellular engineering with non-viral CRISPR technology could be used to replace the genes IL2RA and CTLA4 entirely, which are associated with rare genetic diseases. Scientists have previously shown that they could replace small sections of the IL2RA gene where mutations occur in patients.
However, Marson’s research team demonstrated that with their novel approach, they could replace entire IL2RA and CTLA4 genes at once, allowing them to treat multiple patients with varied mutations, rather than developing personalized templates for each mutation. With almost 90 percent of cells gaining the correct version of the gene through their technique, the researchers are seeking approval to use the approach in clinical trials for CAR-T cell therapy and IL2RA deficiency.









Join or login to leave a comment
JOIN LOGIN