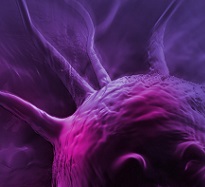
Fibrosis is characterized by excessive deposition of extracellular matrix due to exaggerated repair in response to damage. While the initiating event(s) and underlying pathophysiological processes vary between organs and diseases, common features include the involvement of inflammation, appearance of myofibroblasts, and changes in tissue architecture and function. In lung fibrosis, persistent and non-resolving injury to the alveolar epithelium is thought to drive the disease. The complex interactions between various cell types involved demand state-of-the art in vitro and in vivo models to enable the discovery and development of new drugs for fibrotic diseases.
Charles River has characterized numerous cell-based and animal models of lung fibrosis. In this webinar, we describe the pharmacological characterization of these models, including biomarker profile, histopathological and imaging-based readouts. The extensive data compiled for these models provide a comprehensive platform to first assess lung fibrosis targets and, later, efficacy of prospective anti-fibrotic therapies.
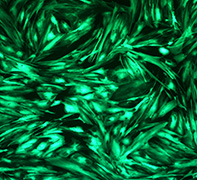
Primary human bronchial epithelial cells and fibroblasts isolated from donors diagnosed with idiopathic pulmonary fibrosis (IPF) and control donors were cultured in 96-well format. Trans-differentiation was induced with TGF-β and assessed by high content imaging (INCell 2200) following immunostaining for fibronectin (EMT in the epithelial cells) and αSMA (FMT in the fibroblasts). The effects of SB525334 (ALK5 inhibitor; assay positive control), pirfenidone, nintedanib, imatinib, MB06322, thalidomide, N-acetyl cysteine, tofacitinib and GSK2126458 were evaluated
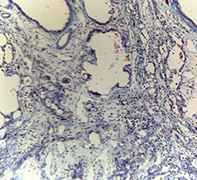
Lung fibrosis was induced in vivo using bleomycin administered to the lungs of both rats and mice and the effects followed for up to 56 days. Key endpoints included changes in body weight, clinical signs, respiratory and lung function parameters, assessment of inflammatory mediators in the BALF, determination of biomarkers in the sera, measurement of collagen deposition (as determined by hydroxyproline determination and imaging of lung tissue), histopathology observed in the lung (graded by Modified Ashcroft score and imaging modalities) and molecular MALDI imaging. The effects of clinically relevant compounds such as nintedanib and pirfenidone have also been investigated.
Both EMT and FMT assays were compatible with high throughput screening of small molecules and RNAi vectors. Signal/background ratio, vehicle tolerance, assay window and intra and inter-assay variability all passed pre-set QC criteria. Nintedanib and GSK2126458 inhibited EMT and FMT. Imatinib and MB06322 inhibited FMT but not EMT. The other compounds did not modulate trans-differentiation (up to 10µM).
Following dosing with bleomycin, multiple lung function parameters were changed, whth peak changes occurring at D14 post-administration. Concomitant with this, was a clear increase in lung inflammation as measured by inflammatory cell infiltrate into the lung. A neutrophilic infiltration was observed which peaked at D14 and recovered by D28. Macrophage numbers continued to increase out to D28. A similar pattern in the BALF was seen for inflammatory mediators such as TNF and KC/GRO. Inflammatory and fibrotic changes at necropsy were consistent with progressive fibrosis, with clear fibrotic lesions apparent from D21 onwards, as well as increases in lung hydroxyproline and collagen deposition. A combination of MALDI imaging and microscopy allowed monitoring the distribution of bleomycin in the lung, as well as the dynamics of (novel) fibrosis markers.
Primary human cell-based assays allow evaluation of compounds targeting various molecular mechanisms. In vivo, the combination of multiple endpoints allows detailed assessment of the potential anti-fibrotic efficacy of both small and large molecules when dosed both therapeutically and prophylactically.
Speakers

Dr. Alan Young, PhD, Business Development Manager, Respiratory Pharmacology, Charles River
Dr. Young joined Argenta, now a Charles River company, in 2011 from AstraZeneca where he had numerous roles including Head of Respiratory Disease Sciences and Director for Early Development Projects. Dr. Young has more than 20 years’ experience in respiratory research ranging from Target Identification/Validation through to Phase III clinical studies. As part of Early Development, he has been responsible for linking Phase IIb clinical studies to pre-clinical endpoints, biomarkers and translational endpoints, and has been responsible for over 20 candidate drugs entering the clinic.

Dr. Jeroen DeGroot, PhD, Director of Cell Biology, Charles River
Dr. DeGroot joined BioFocus, now a Charles River company, in November 2013 as Director of Cell Biology, where he is responsible for target discovery and validation programs as well as phenotypic screening projects across therapeutic areas. Jeroen received his Master’s degree (cum laude) in Biology from the Leiden University and his PhD from the Utrecht University (dept. of Rheumatology) on the molecular mechanisms underlying osteoarthritis. Subsequently he joined the Netherlands Organization for Applied Scientific Research (TNO), where he held various research and management positions over a period of twelve years. Initially he focussed on in vitro and in vivo models as well as translational biomarkers for inflammatory & degenerative diseases. Later, he managed the department of pharmacokinetics and human studies.
During his career Dr. DeGroot has published more than 100 scientific papers, reviews and book chapters, and supervised 6 PhD students. He is member of the American Association of Pharmaceutical Sciences, the Orthopaedic Research Society, the American College of Rheumatology, and the Osteoarthritis Research Society International.

Dr. Vince Russell, PhD, Senior Director of Pharmacology, Discovery Services, Charles River
Dr. Russell has more than 25 years’ experience in Respiratory drug discovery and has been with Argenta, now a Charles River company, for the past 11 years. His current role includes leading, managing and developing the in vivo and in vitro Pharmacology team and capabilities, as well as contributing to all aspects of operations at the Oxford site and presenting our Discovery Services capabilities to clients. During his tenure with the organization, he has also lead teams of various sizes on multiple drug discovery projects with respiratory disease indications.
Dr. Russell joined the company after 13 years with Bayer, where he was responsible for establishing and validating test systems for use in screening cascades and in practical evaluations of new targets. He also contributed significantly to a range of discovery projects including GPCR antagonists, enzyme and ion channel inhibitors.
Who Should Attend?
Senior level professionals from biopharma companies, including the those working in:
- Pharmacology
- Drug Discovery relating to Respiratory Disease
- Pulmonary Disease
- Inflammation & Immunology
Xtalks Partner
Charles River
As your scientific partner and preclinical CRO provider, Charles River provides innovation, flexibility, and efficiency in IND-enabling studies from early discovery research and in vivo pharmacology models through safety assessment. Our unique combination of interdisciplinary, multi-disciplinary drug discovery expertise and unparalleled scope of capabilities in targets, platforms, and therapeutic areas allow us to deliver depth and breadth in science with insight and data you can trust to progress your drug discovery programs at any point along the way, from your very first research question about a molecule to a drug candidates’ first trial in man.
Media Partner
You Must Login To Register for this Free Webinar
Already have an account? LOGIN HERE. If you don’t have an account you need to create a free account.
Create Account