Chiesi Global Rare Diseases in collaboration with Protalix BioTherapeutics announced the US Food and Drug Administration (FDA) approval of their new medication Elfabrio (pegunigalsidase alfa-iwxj) for the treatment of Fabry disease.
Fabry disease, also known as Anderson-Fabry disease, is a rare genetic disorder that falls under the category of lysosomal storage diseases.
Chiesi Global Rare Diseases is a specialized division of the Chiesi Group committed to developing therapies and solutions for individuals affected by rare diseases.
“We established Chiesi Global Rare Diseases to deliver innovative therapies and solutions for people affected by rare diseases. With the FDA approval of Elfabrio, we can now offer people living with Fabry disease an alternative treatment option,” said Giacomo Chiesi, head of Chiesi Global Rare Diseases.
Protalix BioTherapeutics focuses on the production, development and commercialization of recombinant therapeutic proteins.
Dror Bashan, president and CEO of Protalix, further acknowledged that the approval of Elfabrio was made possible due to the extensive collaboration between Chiesi Global Rare Diseases and Protalix BioTherapeutics, as well as the relentless efforts of these two industry-leading companies. He also highlighted that the development of Elfabrio marked a significant milestone in the quest for a durable therapy for Fabry disease, supported by promising results from clinical trials.
About Fabry Disease
Fabry disease, first identified in 1898, is a hereditary deficiency of the enzyme alpha-galactosidase A (alpha-Gal A). This condition arises from mutations in the GAL gene at Xq22, leading to the accumulation of glycosphingolipids within lysosomes in various tissues and organs, such as the heart, kidneys, eyes, vascular endothelium, nervous system and skin. Fabry disease is the only recognized X-linked sphingolipid storage disorder.
The estimated prevalence of Fabry disease in male populations is one in 50,000 males. Since the mutations are located on the X chromosome, males with a single altered copy of the GLA gene in each cell are affected by the condition. In contrast, females, who possess two copies of the X chromosome, may experience milder symptoms or remain asymptomatic due to the presence of one altered copy of the gene.
Classic Fabry disease typically manifests with early symptoms such as chronic neuropathic pain and episodic severe pain crises, resulting from the accumulation of lipids to harmful levels in the body’s autonomic nervous system as a consequence of the gene mutations.
The diagnosis of Fabry disease involves comprehensive assessments of family history, physical examination, clinical and biochemical findings, measurement of alpha-Gal A activity, genetic testing and various imaging procedures. Genetic confirmatory testing is then conducted to identify the specific mutations in the GLA gene.
XTALKS WEBINAR: The Rise of Biologics: Connecting Scientific & IP Insights to Drive Innovation
Live and On-Demand: Wednesday, June 7, 2023, at 10am EDT (4pm CEST/EU-Central)
Register for this free webinar to learn about trends in the global biologics IP landscape, the unique challenges of searching biologics-related IP and more.
How Does Elfabrio Work?
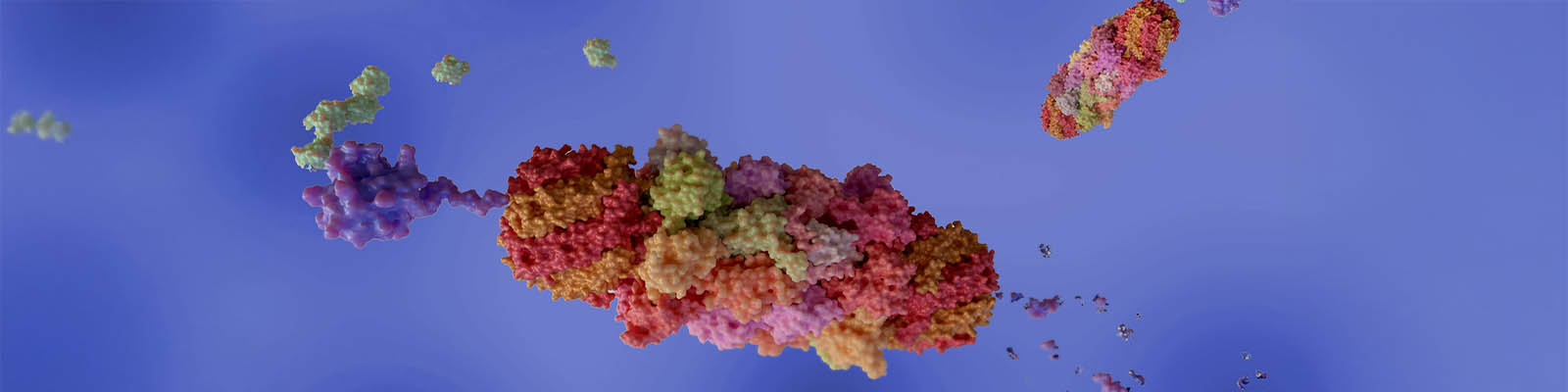
Elfabrio is a hydrolytic lysosomal neutral glycosphingolipid-specific enzyme indicated for the treatment of confirmed Fabry disease in adults. Elfabrio functions as an enzyme replacement therapy, providing an exogenous source of alpha-galactosidase that is deficient in patients with Fabry disease. Upon intravenous infusion, Elfabrio is internalized and transported into lysosomes, where it is believed to exert its enzymatic activity and reduce the accumulation of the fatty substance globotriaosylceramide (Gb3).
Elfabrio is available as a clear and colorless solution in single-dose vials, containing 20 mg/10 mL (2 mg/mL) of pegunigalsidase alfa-iwxj. The administration of Elfabrio is performed by a healthcare professional. The recommended treatment regimen consists of a 1 mg/kg intravenous infusion every two weeks.
Pharmacokinetic studies have demonstrated that following intravenous infusion of Elfabrio at a dose of 1 mg/kg every two weeks, the mean maximum concentration (Cmax) ranged from 21.2 to 23.3 μg/mL, and the mean area under the concentration-time curve (AUCtau) ranged from 958 to 1074 μg·h/mL. The initial half-life of Elfabrio was determined to be 78.9 ± 10.3 hours.
Safety and Efficacy of Elfabrio
The safety and efficacy of Elfabrio have been extensively investigated in comprehensive clinical trials, yielding promising results.
In an open-label, dose-ranging Phase I/II trial involving 14 adults (eight males and six females) diagnosed with Fabry disease, a significant reduction in Gb3 inclusions per renal peritubular capillary (PTC) was observed in renal biopsy specimens after 26 weeks of Elfabrio treatment.
Furthermore, a randomized and active-controlled Phase III trial comprising 77 patients with Fabry disease contributed to the FDA approval. The primary efficacy endpoint was the annualized rate of change in estimated glomerular filtration rate (eGFR) assessed over 104 weeks. Here Elfabrio demonstrated non-inferior efficacy to agalsidase beta (Sanofi Genzyme’s Fabrazyme) in controlling the decline of eGFR. The estimated mean eGFR slope on Elfabrio was -2.4 mL/min/1.73 m2/year, comparable to -2.3 mL/min/1.73 m2/year on agalsidase beta.
Notably, Elfabrio exhibited good tolerability, supporting its potential as a long-term therapy option. The most commonly reported adverse reactions include infusion-associated reactions, nasopharyngitis (common cold), headache, diarrhea, fatigue, nausea, back pain and sinusitis. Although one severe hypersensitivity reaction case was observed in a patient following the initial infusion of Elfabrio, the overall benefits of the drug in treating Fabry disease outweigh the associated risks.
What is the Price of Elfabrio?
The pricing for Elfabrio has not yet been determined; however, it is worth noting that the existing treatment options available for Fabry disease on the market can cost more than $300,000 annually.
Galafold (migalastat), developed by Amicus Therapeutics, was the first oral medication approved by the FDA for the treatment of Fabry disease. Amicus Therapeutics has listed the price of Galafold at approximately $315,000 per year. Fabrazyme is estimated to cost around $340,000 per year for adults. It is important to note that coverage for both Galafold and Fabrazyme may be available through major insurance plans, subject to medical necessity and specific insurance policies.
More Drugs for Fabry Disease Are on the Way
Sangamo Therapeutics, a biotech company headquartered in California, has reported promising results for their gene therapy product candidate, isaralgagene civaparvovec (ST-920), intended for the treatment of Fabry disease. The Phase I/II study involving 13 patients over a period of two years demonstrated a remarkable 78 percent clearance of Gb3 substrates at the six-month mark. Encouraged by these positive outcomes, the company plans to launch a Phase III trial by the end of 2023 to further assess the efficacy and safety of ST-920.
Another potential treatment under clinical investigation for Fabry disease is venglustat malate (GZ-402671), an oral glucosylceramide (GL-1) synthase inhibitor (GCSi) in development by Sanofi Genzyme. Venglustat reduces the production of GL-1 by inhibiting the enzymatic conversion of ceramide to GL-1, consequently reducing the accumulation of glycosphingolipids. A 26-week open-label Phase II study demonstrated that venglustat was well tolerated, with mostly mild adverse events reported. Notably, the study showed a significant reduction in the accumulation of major glycosphingolipids, supporting the effectiveness of venglustat in glycosphingolipid clearance. Furthermore, patients did not exhibit any disease progression during a three-year follow-up period.
Two Phase III clinical trials are currently recruiting patients to further assess the safety and efficacy of venglustat in adults with Fabry disease.











Join or login to leave a comment
JOIN LOGIN