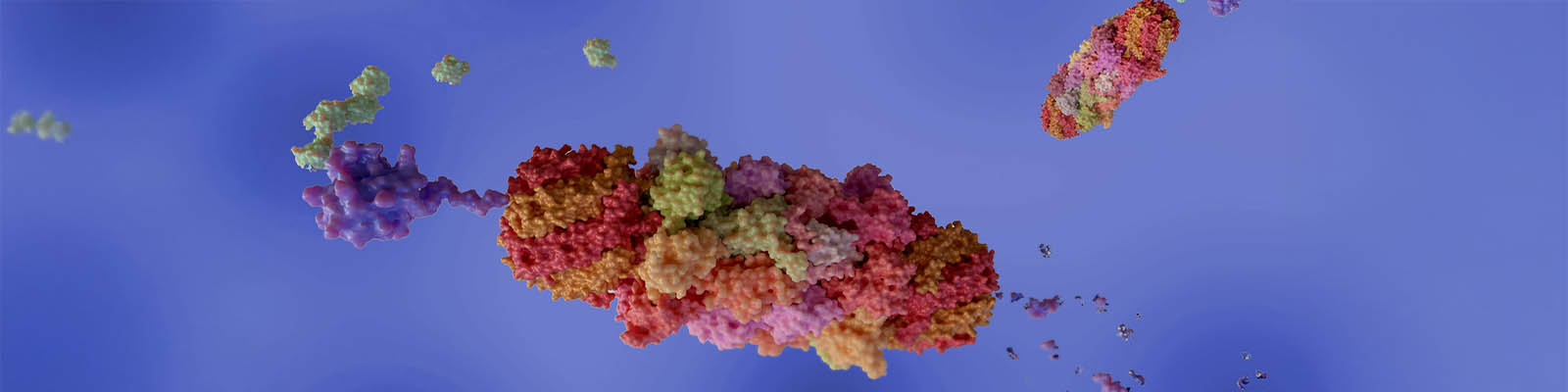
Dual-function fusion proteins represent a cutting-edge approach in biopharmaceutical research, offering a promising avenue for the development of novel therapeutics in the treatment of complex diseases such as cancer and autoimmune disorders. These innovative molecules are engineered by combining two or more functional domains from different proteins into a single, cohesive unit, enabling them to perform multiple biological activities simultaneously.

CEO and Co-Founder of Shattuck Labs
Founded in 2016, Shattuck Labs has quickly distinguished itself through its pioneering approach to developing dual-function fusion proteins for the treatment of cancer and autoimmune diseases. At the helm of this venture is Dr. Taylor H. Schreiber, MD, PhD, CEO and Co-Founder of Shattuck Labs, whose leadership has been instrumental in steering the company toward its mission of creating transformational investigational drugs.
Under Dr. Schreiber’s leadership, Shattuck Labs has made significant strides in the field of cancer immunotherapy. The company’s mission to enhance the efficacy of current treatments through its novel therapeutic approach has the potential to significantly increase response rates, offering new hope to patients with limited options. Their proprietary Agonist Redirected Checkpoint (ARC) platform technology, with its innovative dual-function fusion proteins, exemplifies Shattuck’s commitment to addressing the complexities of immune system modulation in cancer and autoimmune diseases.
Xtalks spoke with Dr. Schreiber about the company’s innovative strategies and scientific foundation underpinning their investigational therapies, and more.
Can you share your journey leading up to your role at Shattuck Labs and how your previous experiences have shaped your vision for your company?
Dr. Schreiber: My path to Shattuck Labs started at a young age. My initial exposure to medicine came through bench research. During high school, I spent three summers as a lab tech in a chronic kidney disease lab. And then I worked in a bone marrow transplant lab during summers in college. My mentor, Dr. Robert Sackstein, played an important role in guiding my career, offering me independence in my research projects.
This experience led me to a combined MD-PhD program at the University of Miami, as I was drawn by the hands-on medical training and the robust research environment. During my PhD, I worked in Dr. Eckhard R. Podack’s lab where I gained exposure to biotech startups, learning about company formation and on serving biotech entrepreneurship.
However, my journey took a turn when I was diagnosed with Hodgkin’s lymphoma during my PhD. After recovering, I realized my potential to impact more lives through research rather than traditional clinical practice.
Post-recovery and after medical school, I joined Heat Biologics as the Chief Scientific Officer. There, I helped diversify the company beyond cancer vaccines, leading to the foundational ideas for Shattuck Labs.
Tell us about Shattuck’s mission and the therapeutic approach.
Dr. Schreiber: Shattuck Labs is dedicated to enhancing cancer immunotherapy outcomes. Recognizing the limited efficacy of existing treatments like Keytruda, which greatly benefit only 20 to 30 percent of patients, our mission revolves around surpassing this therapeutic ceiling. We aim to combine immune checkpoint inhibition, which removes the “brakes” on immune responses, with activation of the same immune system, potentially increasing response rates significantly.
“We were the first to pioneer drugs with this novel configuration and successfully navigate the complexities of their manufacturing.”
– Dr. Schreiber
Our innovative approach involves developing multifunctional molecules capable of both inhibiting immune checkpoints and activating co-stimulatory receptors within the TNF superfamily, which requires a unique trimeric structure, unlike conventional antibodies. We pioneered a novel drug design, akin to a kayak paddle, to achieve this dual functionality and overcome structural challenges, marking an advancement in the field of immunotherapy.
Could you explain the proprietary Agonist Redirected Checkpoint (ARC) platform technology? How is your lead program differentiated?
Dr. Schreiber: Our proprietary Agonist Redirected Checkpoint (ARC) platform technology produces dual-function fusion proteins. Our leading compound, SL-172154, exemplifies this approach. One end of SL-172154 inhibits the CD47 checkpoint on macrophages, preventing the signal cancer cells emit to evade immune destruction. The other end activates the CD40 receptor, enhancing the immune system’s ability to fight cancer. This combination aims to increase both the response rate and the duration of these responses in patients.
SL-172154 entered clinical trials in mid-2020, following promising preclinical results. It’s distinct from other CD47 inhibitors, like magrolimab by Forty Seven Inc., which Gilead acquired for nearly $5 billion after demonstrating significant efficacy in lymphoma and myeloid leukemia. Unlike magrolimab, which was linked to severe anemia due to its FC domain, SL-172154 was designed with an inactive FC domain to avoid this toxicity.
Our approach not only mitigates the risk of anemia but also incorporates the CD40 ligand to potentially enhance the therapeutic effects. Preclinical comparisons with magrolimab showed our drug had higher response rates and longer-lasting effects. This differentiation underscores our commitment to developing safer, more effective treatments for patients.
Can you discuss your therapeutic focus and the clinical applications for this program?
Dr. Schreiber: Our therapeutic focus began with ovarian cancer due to its high CD47 expression, macrophage infiltration and significant unmet medical need, making it a prime candidate for our lead drug, SL-172154. This drug’s efficacy hinges on combination therapy, particularly with treatments that induce pro-phagocytic signals in cancer cells.
We chose to combine SL-172154 with approved chemotherapies and AbbVie’s mirvetuximab, which recently gained approval for platinum-resistant epithelial ovarian cancer patients. Our preclinical data suggest that combining SL-172154 with mirvetuximab could potentially benefit a larger patient group.
Additionally, we targeted acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) to validate our drug in areas where CD47 inhibitors have shown promise. This strategy aimed to establish our drug’s efficacy relative to existing treatments. Despite the competitive landscape in AML and MDS, the discontinuation of other CD47 inhibitors due to toxicity issues has positioned SL-172154 favorably, with early clinical data supporting its efficacy and safety in both ovarian cancer and hematological malignancies. This development presents a unique opportunity for SL-172154 to lead in these therapeutic areas without the associated toxicities that have hampered other programs.
What are key takeaways from the recently presented AML data at the American Society of Hematology Annual Meeting? Can you walk us through upcoming milestones for this program in 2024?
Dr. Schreiber: At the recent American Society of Hematology Annual Meeting, we shared promising data from our Phase I trials on SL-172154 in relapsed refractory AML and MDS patients. Notably, we did have a monotherapy responder who was a relapsed refractory AML patient who responded very quickly, was taken to transplant, and remains cancer-free today. Additionally, our combination therapy with azacitidine, a standard care chemotherapy, showed well-tolerated dose escalation without significant toxicities or anemia, highlighting SL-172154’s potential synergy with existing treatments.
Looking ahead to 2024, we’re excited to expand our AML and high-risk MDS studies. Mid-year, we aim to present data on complete response rates and response durability from these expanded cohorts. This will offer deeper insights into SL-172154’s efficacy, particularly in TP53 mutant AML patients and high-risk MDS patients, where early results have already surpassed expectations. Success in these metrics could propel SL-172154 into Phase III trials, marking a significant leap towards potential approval and a transformative impact on patient care in these challenging conditions.
What are the key takeaways from the platinum-resistant ovarian cancer (PROC) data, and can you walk us through upcoming milestones and catalysts for this program?
Dr. Schreiber: In our platinum-resistant ovarian cancer (PROC) program, we’ve completed enrollment for the cohort combining our drug with pegylated liposomal doxorubicin. By mid-year, we’ll report on both complete and partial response rates, along with response durability. For clinical significance, we’re aiming for an objective response rate of at least 25 percent, with a progression-free survival (PFS) of five months or more.
Additionally, we’re progressing with the second combo cohort in collaboration with ImmunoGen, now part of AbbVie. We anticipate completing enrollment approximately 70 patients and will share objective response rates and response durability insights in the second half of the year.
Our upcoming milestones include revealing critical data points by mid-year and in the latter half, which will guide our next steps in advancing this promising treatment for PROC. Collaborating with AbbVie, we’ll strategize the optimal way to disclose these findings, marking significant catalysts for our program.
As Shattuck Labs continues to advance its product candidates through global clinical trials, Dr. Schreiber’s insights into the company’s journey, mission and groundbreaking ARC platform technology provide a compelling narrative of innovation and hope. His vision for Shattuck Labs not only underscores the company’s commitment to scientific excellence but also reflects a broader aspiration to redefine the landscape of therapeutic interventions for some of the most challenging diseases facing humanity today.










Join or login to leave a comment
JOIN LOGIN