Researchers at Duke University have found an area in the brain of mice that can suppress pain. Their findings come from work in which they were trying to understand the mechanisms of general anesthesia in pain suppression, which is separate from the loss of consciousness that it induces.
The area was found to be located in the amygdala, which makes the discovery surprising because this brain structure is involved in the processing of emotional responses such as fear, anxiety and aggression – including the flight or flight response – as well as memory and decision-making. However, the Duke University research team’s findings shed light on how the amygdala may also control pain processing.
In speaking about the findings, lead author on the study Dr. Fan Wang, the Morris N. Broad Distinguished Professor of Neurobiology in the School of Medicine at Duke University, said, “People do believe there is a central place to relieve pain, that’s why placebos work… The question is where in the brain is the center that can turn off pain.”
The study was published in the journal Nature Neuroscience.
Related: Researchers Identify Eye Signals That Prevent Circadian Rhythm Shifts
Wang’s research lab has long been interested in investigating how neuronal networks in the brain regulate pain in the body. In fact, their latest work follows up on a 2019 study, also published in the journal Nature Neuroscience, in which they found that general anesthesia activates the supraoptic nucleus of the brain to promote slow-wave sleep.
However, sleep and pain are different, which is what prompted the researchers to further explore how pain is specifically regulated under anesthesia. While research on the subject of pain has typically involved examining neurons that activate pain pathways, Wang and her team’s new research findings have uncovered a class of neurons that can turn them off.
“Most of the previous studies have focused on which regions are turned ON by pain,” Wang said. “But there are so many regions processing pain, you’d have to turn them all off to stop pain. Whereas this one center can turn off the pain by itself.”
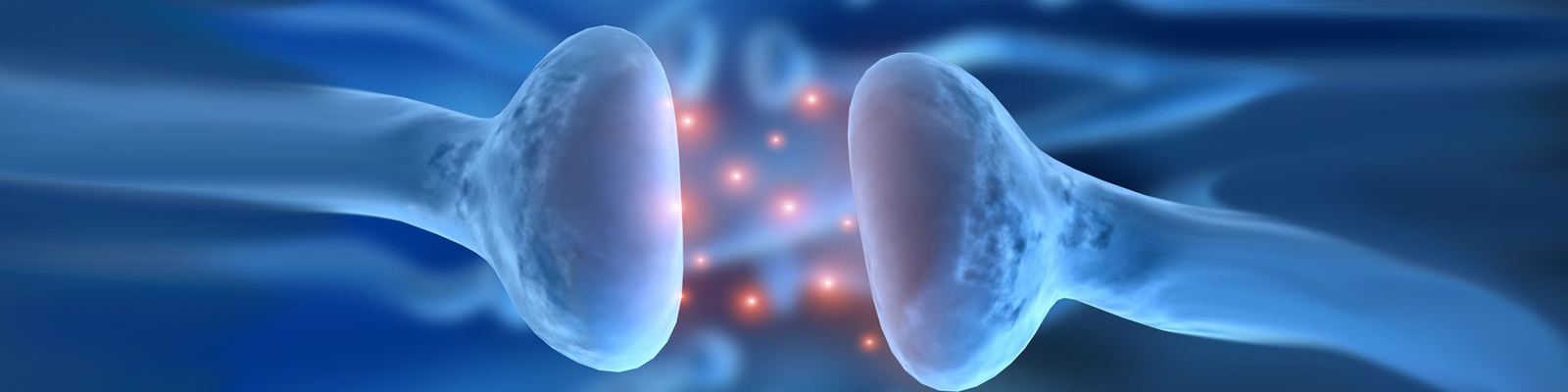
The researchers discovered that general anesthesia activates a specific subset of inhibitory GABAergic neurons (neurons that produce the inhibitory neurotransmitter GABA) in the central amygdala, which they termed the CeAga neurons (‘CeA’ stands for central amygdala, while ‘ga’ refers to activation by general anesthesia).
Despite the fact that compared to humans, mice generally have a relatively large central amygdala, Wang said she had no reason to think we have a different system for controlling pain.
Using pioneering techniques developed by Wang and her team of researchers, including in vivo calcium imaging to track the paths of activated neurons in mice, the researchers found that different general anesthesia drugs activate a shared collection of CeAGA neurons.
By giving mice a mild pain stimulus, the researchers were able to map all of the pain-activated brain regions. These regions represented 16 centers within the central amygdala that were able to receive inhibitory input from the CeAga.
“Pain is a complicated brain response,” Wang said. “It involves sensory discrimination, emotion, and autonomic (involuntary nervous system) responses. Treating pain by dampening all of these brain processes in many areas is very difficult to achieve. But activating a key node that naturally sends inhibitory signals to these pain-processing regions would be more robust.”
When a mouse feels uncomfortable, it exhibits ‘self-caring’ behaviors such as paw-licking or face-wiping. The researchers found that by activating the CeAGA neurons using a technology called optogenetics, in which light is used to activate a specific population of cells, these behaviors were completely eliminated.
Wang said that the moment the light was switched on to activate the anti-pain center, the paw-licking or face-wiping behaviors were “completely abolished” and that it was “so drastic… they just instantaneously stop licking and rubbing.” Activation of CeAGA neurons thus suppressed both reflexive and self-recuperating behaviors in response to pain, and inhibited neuropathic pain-induced mechanical hyper-sensitivity.
On the other hand, when the activity of these CeAGA neurons was inhibited, the mice experienced intense pain in response to temporary insult. It also negated the effects of low-dose ketamine, an anesthetic drug that allows sensation but blocks pain, through activation of the CeAga pain center, which it required for its action.
Overall, it was observed that the CeAGA neurons possessed basal activity, which was generally reflective of an animal’s internal state rather than the external stimuli it was subjected to.
With these results, the researchers now hope to find drugs that can act as potential pain killers by targeting these inhibitory pain neurons to suppress pain. In aims of finding specific targets in the specialized neurons, Wang explained that, “The other thing we’re trying to do is to (transcriptome) sequence the hell out of these cells.” This will allow for the identification of relevant genes or cell surface receptors among this specific subset of neurons that can be targeted with a drug to activate them in order to relieve pain.





Join or login to leave a comment
JOIN LOGIN