Myelodysplastic syndromes (MDS) are a group of clonal hematopoietic disorders marked by ineffective blood cell production, progressive cytopenias and the risk of transformation to acute leukemia. In the US, roughly 10,000 to 15,000 new cases are diagnosed each year (with an age-adjusted incidence of ~4.4–4.6 per 100,000).
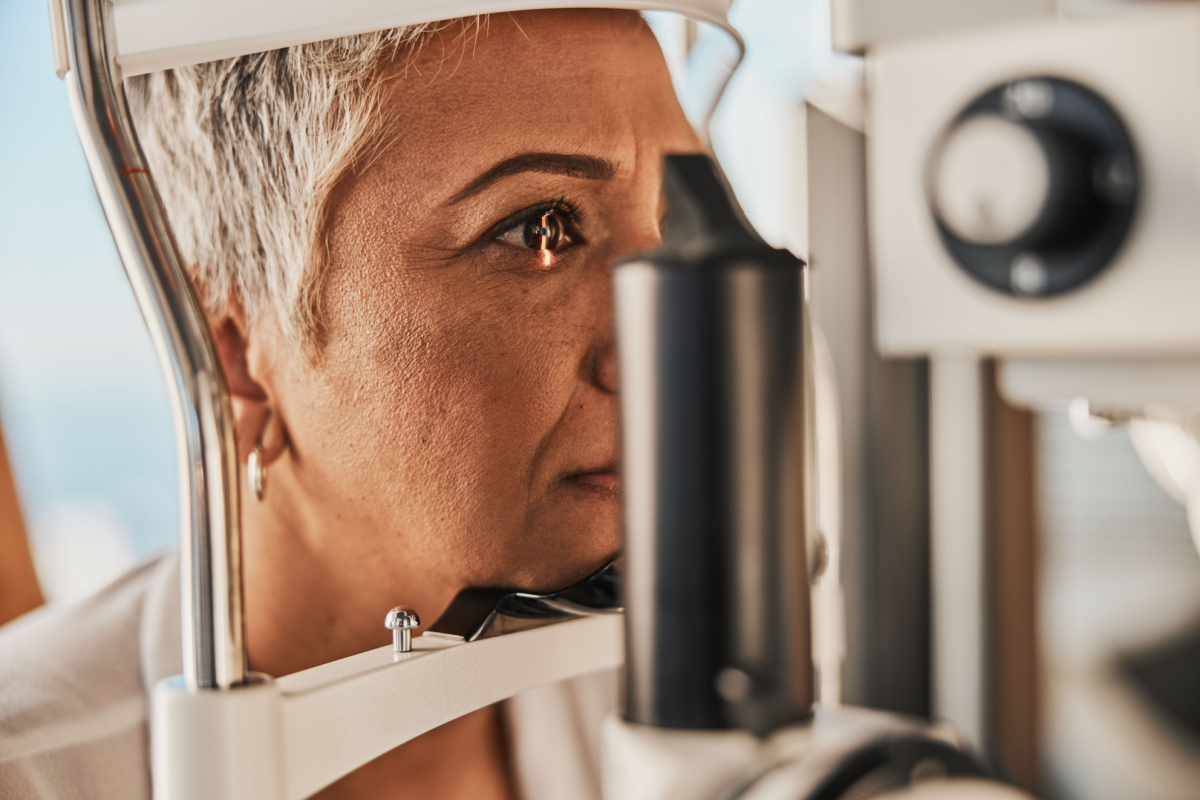
MDS is primarily a disease of older adults: the median age at diagnosis is around 70 years, and incidence rises steeply with age, affecting more than 25 per 100,000 in populations older than 65. Prognosis remains poor: the observed three-year survival rate is about 42%, dropping to 29% at five years, depending on risk stratification.
Amid limited treatment options and high relapse rates, Faron Pharmaceuticals is advancing a novel investigational monoclonal antibody-based immunotherapy for MDS treatment that targets the tumor microenvironment rather than the cancer cells alone.
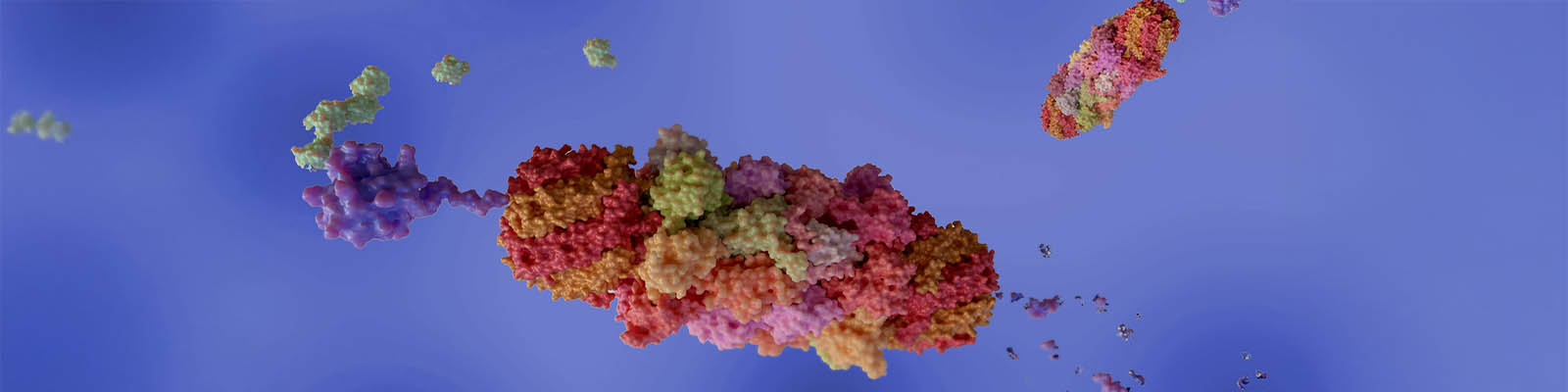
The investigational drug targets CLEVER-1, a scavenger receptor on macrophages that promotes immune suppression within the bone marrow. By blocking this receptor, the treatment reprograms macrophages into a pro-inflammatory state capable of supporting anti-tumor immune activity.

Chief Medical Officer
Faron Pharmaceuticals
Faron’s lead candidate also aims to restore normal immune activation, strengthening T-cell responses and enabling the patient’s immune system to target malignant cells more effectively. It represents a promising new direction in the treatment of higher-risk MDS.
Dr. Petri Bono, Chief Medical Officer at Faron Pharmaceuticals, draws on decades of clinical and research experience to rethink how MDS is studied and treated. In our interview, he outlines how advances in genomics, immune microenvironment biology and smarter trial design are converging to redraw what’s possible in this challenging space.
Over the last ten years, MDS biology has moved from descriptive morphology to molecular precision. Dr. Bono attributes much of that shift to comprehensive genomic profiling and next-generation sequencing (NGS).
“These technologies have dramatically increased our understanding of the mutational landscape of the disease,” he explained.
NGS has identified recurring genetic mutations in MDS, helping researchers distinguish which mutations drive disease progression and which are incidental, and revealing how specific genetic changes influence clinical outcomes.
These molecular findings have been translated into practical clinical tools, including the 2022 IPSS-M (International Prognostic Scoring System-Molecular), an updated scoring system that incorporates genetic mutation data alongside traditional clinical and cytogenetic measures. Dr. Bono noted that precise baseline characterization using such models is essential for fair randomization and meaningful outcome interpretation in clinical trials.
“MDS has been shifting from a morphology- or cytogenetic-defined disease to a molecularly defined one.”
— Dr. Petri Bono
Another key advance is single-cell longitudinal sequencing, which allows researchers to observe clonal evolution and resistance mechanisms in real time. “It helps to understand better how clones expand and how these diseases actually progress,” Dr. Bono said.
Among the most critical discoveries is the behavior of TP53 mutations. Multi-hit, or biallelic, TP53 alterations define an especially aggressive patient subset with short-lived responses despite initial sensitivity to treatment. “In future trials, at least stratification, and perhaps even dedicated studies, for TP53-mutated MDS will be important,” he added.
Beyond genomics, scientists are uncovering the role of immune dysregulation within the bone-marrow microenvironment. Elevated inflammatory signaling and suppressive macrophage activity promote disease progression.
“Immune suppression is the reason these diseases can progress to a more malignant phenotype,” Dr. Bono said, noting that reprogramming macrophages toward a pro-inflammatory state could restore antitumor immunity.
Read Xtalks Clinical Edge™ Issue 6 Featuring Faron Pharmaceuticals and More
Xtalks Clinical Edge is a magazine for clinical research professionals and all who want to be informed about the latest trends and happenings in clinical trials. This magazine immerses you in a world where industry leaders, patient advocates and top researchers converge to provide the most insightful perspectives on clinical trials.
Immunotherapies and Myeloid-Targeted Strategies
Standard treatment for MDS still relies mainly on hypomethylating agents, but their limitations have spurred exploration of new immune-modulating combinations.
According to Dr. Bono, the field is seeing “huge potential by combining new agents with hypomethylating agents and novel immunotherapies, including those targeting CD47, TIM-3, bispecific molecules and myeloid cell antigens.”
Some trials with earlier immunotherapy targets have fallen short in Phase III settings, often due to narrow designs or safety issues, yet the lessons learned are driving better-informed strategies. The next generation of immunotherapies, he said, aims to reverse immune suppression rather than induce broad cytotoxicity, potentially improving both safety and durability.
Myeloid-reprogramming approaches are of particular interest because they act on the tumor microenvironment. By shifting macrophages from an immunosuppressive (M2-like) state toward a pro-inflammatory (M1-like) phenotype, these therapies may enhance the immune system’s natural antitumor response and restore hematopoietic balance.
Achieving higher rates of complete remission (CR) is an important step toward potentially curative outcomes in MDS. Deeper remissions improve patients’ eligibility for stem-cell transplantation, which is the only treatment currently considered curative. Dr. Bono explained that in recent immune-based therapy trials, a notable proportion of patients who were initially ineligible for transplant later became eligible after responding to treatment.
He also highlighted bispecific agents that recruit immune effectors directly against myeloid antigens such as CD3, CD33 or CD123. “They’re mostly in early-phase development,” he said, “but they’re very much interesting to the scientific community at the moment.”
Tackling Resistance and Improving Outcomes
Drug resistance remains one of the most persistent barriers to improving long-term outcomes in MDS.
Standard therapies, such as hypomethylating agents, often lose effectiveness after several treatment cycles as malignant clones adapt and new mutations emerge.
“With the standard of care, patients become refractory quite fast,” Dr. Bono said. Overcoming this challenge, he explained, requires a deeper understanding of the biological diversity within MDS, including high-risk molecular subtypes such as TP53-mutated disease, and the design of combination strategies that can target multiple pathways or immune mechanisms simultaneously to delay or prevent resistance.
Beyond extending survival, Dr. Bono emphasized that effective disease control must also translate into a better quality of life. “Quality of life means less anemia, less weakness, less bleeding, fewer infections, fewer hospitalizations,” he said.
Regulators are increasingly recognizing these measures as meaningful endpoints alongside overall survival, reflecting a broader shift toward evaluating how therapies help patients live better, not just longer.
Designing Trials with Patients in Mind
For Dr. Bono, patient-centricity must move beyond rhetoric. “We need to have endpoints in the trial that are aligned with the impact on the daily life of the patients,” he said.
Integrating patient advisory boards early in protocol development helps ensure trials reflect real patient priorities.
Transparency and feedback loops are equally important. “It’s a slogan, this patient centricity, but I think there are ways to increase it,” he acknowledged, noting that hematology and solid-tumor research alike can benefit from stronger bidirectional communication between sponsors and participants.
More Innovative Recruitment for Rare Cancers
Recruiting patients with rare cancers like MDS requires both community partnership and technical innovation. “Collaboration with patient organizations … is something that traditionally has not been done so much,” Dr. Bono said. Groups such as the MDS Foundation now provide clear information on ongoing trials and eligibility, enabling faster and more inclusive enrollment.
He expects basket and umbrella trial designs to gain ground, especially as molecular heterogeneity replaces histology as the defining enrollment criterion. “MDS is not just one disease,” he explained. “It’s important to try to take into account these kinds of differences.”
Modern trials are also becoming more adaptive, allowing sample-size adjustments based on emerging efficacy data. “This is something that’s also approved by regulatory authorities,” he noted, provided it’s pre-specified in the protocol.
Such flexibility, combined with centralized eligibility review across multi-continental sites, ensures consistency as studies scale to hundreds of locations.
New Endpoints and Evolving Standards
The adoption of the International Working Group 2023 (IWG 2023) response criteria represents a major shift in how clinical benefit is measured in MDS. The new framework moves beyond purely laboratory-based or morphological assessments to focus on outcomes that more accurately reflect a patient’s clinical improvement and daily functioning. “They capture outcomes that are more clinically meaningful and actually more patient-centered than just lab-defined responses,” Dr. Bono said.
Unlike earlier response systems, which mainly recognized full CR, the IWG 2023 criteria acknowledge partial yet clinically significant responses, such as CRh (complete remission with partial hematologic recovery), CRi (complete remission with incomplete marrow recovery) and composite CR categories.
These new definitions better capture meaningful improvements in blood counts and transfusion independence, which are known to correlate with longer survival and improved quality of life. For example, hemoglobin threshold for CR was lowered to 10 g/dL in the IWG 2023 criteria from 11 g/dL in IWG 2006 criteria. The updated criteria also addresses limitations and clarifies response assessments for patients with low baseline blast counts (<5%).
“I’m proud to tell you that we agreed with the FDA that our Phase III will be the first ever prospective randomized MDS trial to use these new criteria [the IWG 2023 response criteria] as the primary endpoint,” Dr. Bono shared.
The agency has endorsed CR plus CR-equivalent as a co-primary endpoint alongside overall survival, signaling a clear move toward regulatory frameworks that prioritize patient-centered and clinically meaningful outcomes.
AI, Digital Tools and Real-World Data
Emerging technologies are reshaping how oncology trials are designed, monitored and analyzed. “AI helps to aid recruitment, standardize assessments and probably personalize a little bit the trial conduct,” Dr. Bono said.
AI can enhance centralized image and pathology review, ensuring consistent eligibility and response evaluation across sites. It can also classify patients more accurately, reducing heterogeneity that has undermined past MDS Phase III studies.
Dr. Bono also discussed the growing conversation around the use of AI-generated comparator arms, which are simulated control groups built from real-world data (RWD) rather than traditional randomized control populations. These so-called synthetic arms use AI and historical patient records to model how individuals might have responded to standard-of-care treatments, potentially reducing the need for large placebo or control cohorts in rare or high-risk diseases like MDS.
While this approach could accelerate trial timelines and reduce patient burden, regulators remain cautious. “Maybe now there’s a trend that AI-based synthetic arms are not enough, that there needs to be also true randomization,” Dr. Bono said.
The concern, he explained, is that even sophisticated modeling cannot fully eliminate selection bias or confounding variables, which randomized studies are designed to control.
Importantly, regulatory agencies on both sides of the Atlantic, including the FDA, EMA and MHRA, are working more closely than ever to harmonize expectations for oncology trial design. “Investigators appreciate that … similar endpoints, patient-centric endpoints, can be included in the trials,” Dr. Bono noted. This alignment supports greater consistency in how emerging methodologies, such as the use of AI, real-world evidence and adaptive designs, are validated and accepted across jurisdictions.
Next Steps for MDS Clinical Research
The MDS field is entering an era defined by molecular precision, immune reprogramming and data-driven trial design.
From genomic profiling to AI-supported analytics, each layer of innovation contributes to more personalized and patient-relevant therapies.
As Dr. Petri Bono summarized, the path forward lies in uniting scientific rigor with empathy: understanding the disease at its molecular level while ensuring that trial design and endpoints reflect what truly matters to patients: living longer and living better.











Join or login to leave a comment
JOIN LOGIN