Cardiovascular diseases are the number one cause of death in the world. According to the World Health Organization (WHO), almost 18 million people died from cardiovascular diseases in 2019, which was 32 percent of all deaths globally.
Cardiovascular stents are expandable, small mesh tubes that are usually put inside a coronary artery to support and open arteries that are weakened or narrowed due to atherosclerosis. Stents help to restore oxygen-rich blood flow to the connected tissues.
There are three main types of coronary or carotid artery stents: bare metal stents, drug-eluting stents that are coated with drugs to be slowly released into the artery to help prevent the artery from clogging again and biodegradable stents for temporary needs.
In addition, stents can be used to treat aneurysms and narrowed airways in the lungs. Stents can be made of metal mesh, silicone, fabric or a combination of materials, depending on their use.
In recent years, there has been an increase in research interest for smart stents, which are stents with integrated sensors. Such devices have a great potential for real-time and continuous monitoring of parameters such as blood pressure and flow. In addition, the monitoring done with smart stents may help prevent some clinical complications of conventional stents, which include stent thrombosis (a life-threatening event where the artery is completely blocked due to the formation of a blood clot in the stent) and in-stent restenosis (a slow re-narrowing of the segment with the stent).
Researchers at the Georgia Institute of Technology have recently developed a new implantable vascular monitoring system consisting of a stent and soft sensors. This device is wireless and batteryless and operates by inductive coupling which allows for wireless energy transfer using magnetic fields.
A study describing this new wireless vascular electronic system was published a week ago in Science Advances. This study was funded with the aid of the National Science Foundation (NSF), the National Institutes of Health (NIH) and the American Heart Association.
XTALKS WEBINAR: Cardiac Safety Solutions in Decentralized Clinical Trials (DCT)
Live and On-Demand: Tuesday, May 24, 2022, at 1pm EDT (10am PDT)
Register for this free webinar to learn how BioTel Research, now part of Philips, is leveraging the 12-lead, at-home, ECG device to provide an integrated, remote monitoring solution designed with the patient in mind while meeting the requirements and flexibility needed by sponsors.
“This electronic system is designed to wirelessly deliver hemodynamic data, including arterial pressure, pulse and flow, to an external data acquisition system, and it is super small and thin, which is why we can use a catheter to deliver it, anywhere inside the body,” said Dr. Woon-Hong Yeo, associate professor of mechanical engineering and biomedical engineering at Georgia Tech and corresponding author of the study, in Georgia Tech’s news release.
The device developed by Dr. Yeo and his research team is truly super small, as seen in the photo below.
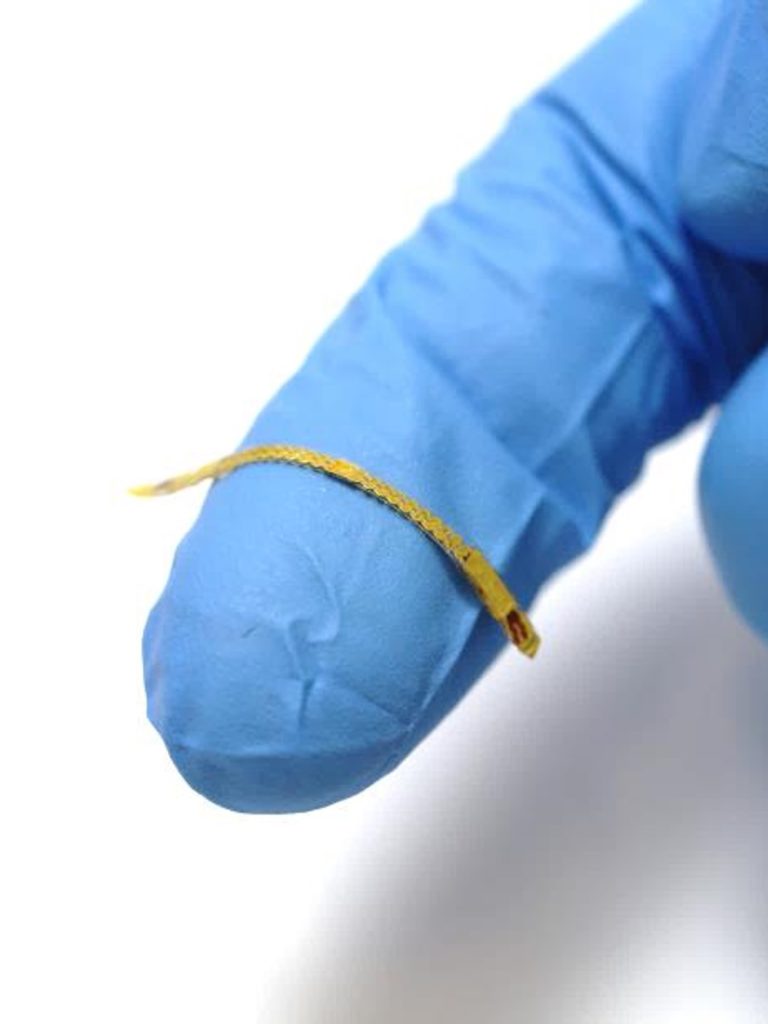
The smart stent developed by Dr. Yeo and his research team is wireless and batteryless. The device delivers hemodynamic data to an external data acquisition system. Photo courtesy of Georgia Institute of Technology.
In their published study, Dr. Yeo and colleagues have validated the wireless electronic system in artery models and conducted a minimally invasive catheter implantation of the smart stent platform in an in vivo animal model.
By providing wireless monitoring of hemodynamics, the long-term goal of this small implantable device is to help monitor treatment and disease progression. Another benefit of the device is that it could evade the need for hemodynamics monitoring methods, such as magnetic resonance imaging (MRI), angiography and Doppler ultrasound, which can monitor parameters only during a limited time frame while the patient is stationary.
“Basically, you can put this sensor system anywhere inside the body. The other thing about this technology platform is, in addition to being an implantable sensor system, it can be used as a wearable system. Think about a smartwatch and how much of its bulk is taken up by circuits or batteries. If you remove all of that, you have a device that is thinner than a typical Band-Aid, an almost invisible health monitor that you can wear anywhere,” said Dr. Yeo in Georgia Tech’s news release.
Dr. Yeo recently got a 3-year, $400,000 grant from the NSF to continue to develop the technology in the field of printed nanomembrane sensors and bioelectronics for wireless and continuous vascular monitoring.











Join or login to leave a comment
JOIN LOGIN