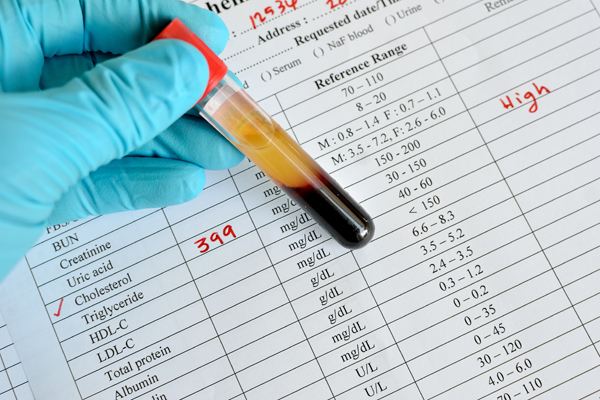
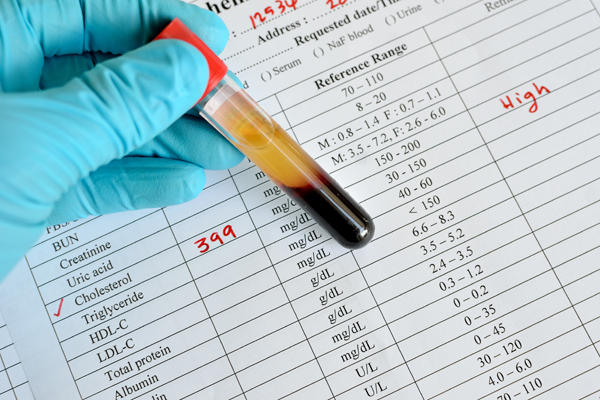
Amgen’s offer to refund payers if patients experience a cardiac event while being treated with their cholesterol drug Repatha (evolocumab), isn’t doing much to improve the cost-effectiveness of the PCSK9 inhibitor, according to a new study published in the Annals of Internal Medicine. Despite the fact that Amgen has provided clinical evidence to back up its cardio-protective claims for Repatha in patients with atherosclerotic cardiovascular disease (ASCVD), insurance coverage and uptake of the drug has been less impressive than expected, due in part to its hefty $14,000 per-year price tag.
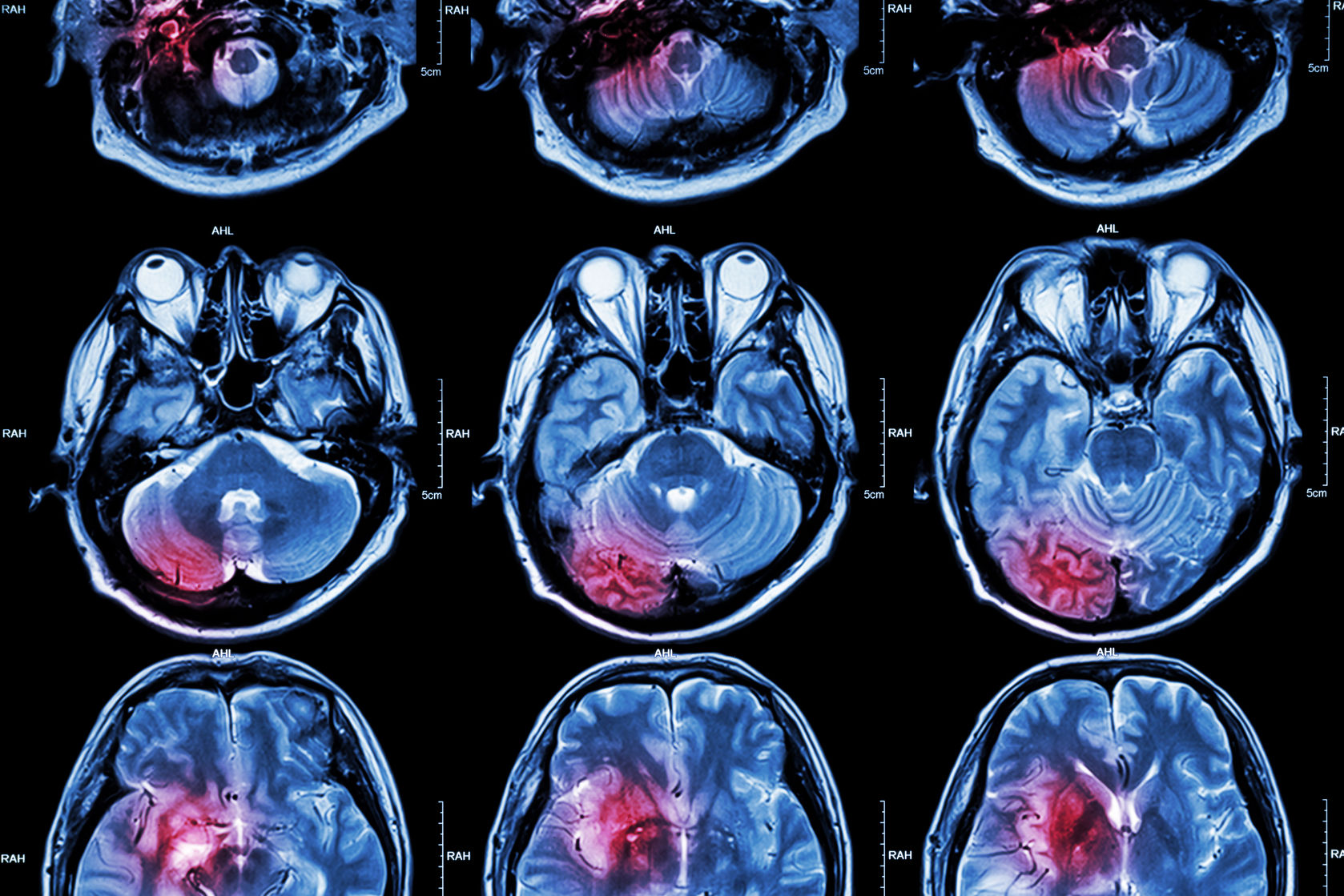
In 2017, Amgen reported results from their nearly 30,000 patient FOURIER trial which established that Repatha was able to reduce a patient’s risk of suffering a major cardiovascular event – such as first heart attack, stroke or cardiovascular death – by 20 percent, when used in combination with statin therapy. Bolstered by this data, Amgen sought to make coverage of the PCSK9 inhibitor drug more attractive to payers by introducing the money-back guarantee for patients who suffer a heart attack or stroke after at least six months of taking the drug as prescribed.
Now, researchers from the University of California, San Francisco, and the Institute for Clinical and Economic Review (ICER) – a Boston-based non-profit that assesses the value of new drugs – are calling Amgen’s outcome-based pricing model into question. In their study, the research team looked at the incremental cost-effectiveness ratios for PCSK9 inhibitors, and the older cholesterol-lowering drug ezetimibe, in combination with statin therapy.
RELATED: Some Patients Taking Repatha Will Receive Full Refund if They Experience a Cardiac Event
The researchers found that refunding the cost of Repatha as well as any hospital costs related to the patient’s cardiac event would only bump up the drug’s cost-effectiveness ratio by just over three percent. This represents a modest improvement that wouldn’t increase Repatha’s value to justify the $14,000 annual cost of treatment in the eyes of ICER.
The results of the study aren’t necessarily a surprise considering that rates of major cardiac events in the ASCVD patient population are low to begin with. Since patients taking Repatha have an even lower chance of suffering a heart attack or stroke, Amgen will rarely need to issue a refund, impacting the cost-effectiveness of therapy for all patients.
“This feeble effect is a consequence of 2 forces: Evolocumab’s list price of $14, 452 per year was gauged to be more than 3.4-fold its price at conventional cost-effectiveness thresholds, and the frequency of the refund would be driven by the frequency of heart attacks or related cardiovascular events in the target population, which is very low,” said Dr. Sham Mailankody and Dr. Peter B. Bach, two doctors from Memorial Sloan Kettering Cancer Center who were not involved with the research. “Put another way, if evolocumab’s starting price is manyfold greater than it should be, refunds can achieve a reasonable net price only if there are many events that trigger them. If not, the net price (the average price including refunds) will be very close to the starting price.”
Despite the criticism, Amgen has remained adamant that their outcomes-based pricing model is good for patients and payers and has recently highlighted the risks of denying access to PCSK9 inhibitors to patients with cardiovascular disease. In March, they shared data from a study presented at the American College of Cardiology’s 67th Annual Scientific Session that found over 110,000 cardiovascular events each year could occur in patients denied access to Repatha.
“These data further highlight what we have seen for the past two years and the need for improved access to medications like Repatha that reduce life-changing events, such as heart attacks and strokes, among high-risk cardiovascular patients,” said Dr. Sean E. Harper, executive vice president of Research and Development at Amgen. “Clinical data and experience tell us those at highest risk for further cardiovascular events benefit the most from intensive LDL-cholesterol lowering with a PCSK9 inhibitor, like Repatha. We are in active discussions with payers to align on clinically grounded, utilization management policies with the goal of best serving the needs of appropriate patients and ensuring access to Repatha.”




Join or login to leave a comment
JOIN LOGIN