While immunotherapies have revolutionized cancer treatment in recent years, they often fall short in the most aggressive and treatment-resistant malignancies. Glioblastoma, pancreatic cancer and refractory melanoma — among the deadliest and most complex cancers — continue to present major challenges in oncology.
Glioblastoma is the most common malignant brain tumor in adults, with approximately 14,000 new cases diagnosed annually in the US. Despite standard treatments including surgery, radiation and chemotherapy, the median survival is only 12 to 15 months, and the five-year survival rate hovers between 5% and 10%.
Pancreatic cancer fares little better, ranking as the third leading cause of cancer-related death in the US, with a five-year survival rate of just 12% and more than 64,000 new diagnoses each year.
Refractory melanoma — defined by resistance to checkpoint inhibitors — remains difficult to treat, with limited options and poor patient outcomes despite recent advances.
These difficult-to-treat cancers are where Diakonos Oncology, a Houston-based biotech company, is aiming to make a difference. Focused on advancing a novel dendritic cell therapy platform, Diakonos is developing a tumor-agnostic approach designed to activate the immune system in a more natural, robust way than conventional therapies.
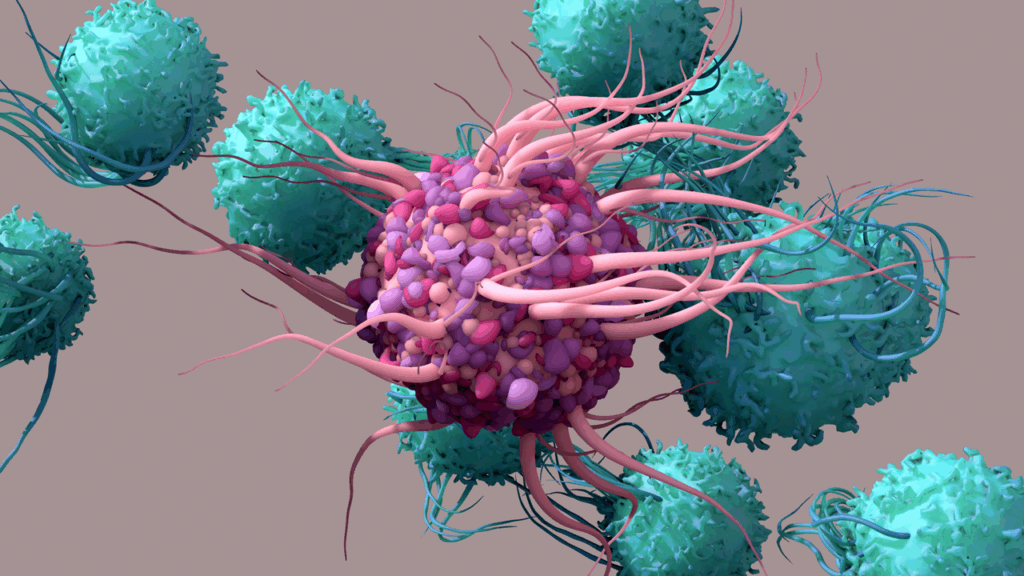
Dendritic cells are professional antigen-presenting cells that serve as key initiators of T-cell responses, but have historically been underutilized in cancer immunotherapy compared to more established approaches like CAR T-cell therapy.

President and Chief Operating Officer
Diakonos Oncology
Diakonos’ proprietary “double-loading” technique stimulates a previously undiscovered pathway for viral recognition and immune response. By loading tumor-derived material both internally and externally into a patient’s own dendritic cells — white blood cells that naturally detect threats — the approach mimics the simultaneous signaling seen during a viral infection, triggering a broad and potent immune activation without the need for viral vectors or genetic engineering.
With the global cell therapy market projected to reach $36 billion by 2033, most commercial activity has focused on CAR T therapies. However, growing interest in alternative cell therapy platforms, including dendritic cells, natural killer (NK) cells and tumor-infiltrating lymphocytes (TILs), is reshaping the landscape. Diakonos is at the forefront of this shift, targeting cancers with the fewest therapeutic options and pushing the boundaries of personalized immunotherapy.
Jay Hartenbach, President and Chief Operating Officer (COO) of Diakonos Oncology, discussed how the company’s dendritic cell platform is designed to overcome longstanding limitations in cancer immunotherapy, both scientifically and operationally.
Xtalks Clinical Edge™: Issue 5 — Diakonos Oncology’s Innovation in Dendritic Cell Therapy for Hard-to-Treat Cancers
Xtalks Clinical Edge™ is a magazine for clinical research professionals and all who want to be informed about the latest trends and happenings in clinical trials. This magazine immerses you in a world where industry leaders, patient advocates and top researchers converge to provide the most insightful perspectives on clinical trials.
Rewiring the Immune Response with Dendritic Cell Therapy
Most immunotherapies on the market today, such as checkpoint inhibitors and CAR T-cell therapies, focus on targeting known tumor antigens or engineering T cells to recognize specific markers. Diakonos takes a different route. The company uses a patient’s own dendritic cells — which naturally alert T cells to potential threats — and loads them with tumor-specific material to train the immune system to recognize and destroy cancer.
What sets the company apart is its “double-loading” technique. Each patient’s dendritic cells are exposed to both lysate (a mixture of tumor proteins) and tumor-derived mRNA. The mRNA is loaded internally, while the lysate is applied externally. This dual delivery simulates a viral infection, amplifying the immune response.
“Our bodies have evolved over millions of years to detect and respond to viral threats,” said Hartenbach. “By replicating that mechanism, we’re helping the immune system recognize cancer as something it should act against.”
This strategy allows the immune system to see the complete antigenic profile of the tumor, rather than a single mutated protein. It also simplifies manufacturing by eliminating the need for viral vectors or genetic modification. From a patient perspective, the therapy does not require lymphodepleting chemotherapy or hospitalization, making it less burdensome than traditional cell therapies.
Pursuing the Most Challenging Indications
Rather than starting with a more common or less aggressive cancer, Diakonos deliberately chose to test its platform in glioblastoma, one of the most difficult cancers to treat. Glioblastoma is characterized by high tumor heterogeneity, limited resectability and a notoriously resilient microenvironment protected by the blood-brain barrier.
“It’s somewhat unique for an early-stage cancer immunotherapy company to go after arguably one of the most difficult indications. But we saw glioblastoma as a way to quickly determine if the therapy could make a difference.”
— Jay Hartenbach
Following a successful Phase I trial, the company opened a Phase II study in early 2025 and began enrolling patients across multiple US sites. Early interest from leading academic centers has helped Diakonos accelerate this expansion.
In parallel, the company launched a Phase I trial in pancreatic cancer and plans to initiate a refractory melanoma trial later this year. These cancers, while biologically distinct, share two key characteristics: they’re aggressive, and they lack effective treatment options.
A Consistent, Tumor-Agnostic Platform
Despite the variation in tumor biology, Diakonos’s approach is consistent across indications. Once a tumor sample is collected, the company isolates the lysate and mRNA, loads them into the patient’s own dendritic cells and returns the cells for injection. The only logistical differences are the site of tumor collection and administration.
This tumor-agnostic consistency offers scalability, allowing Diakonos to expand its platform across multiple cancers without altering its core manufacturing process.
“You don’t need this kind of approach for early-stage prostate cancer,” Hartenbach said. “But for late-stage diseases with few options, we believe this personalized model makes sense.”
The company is exploring additional applications in ovarian and renal cell cancers, both of which represent underserved populations in the immunotherapy landscape.
Strategic Trial Design and Real-World Complexity
To meet regulatory expectations and practical constraints, Diakonos has adopted hybrid clinical trial designs. In the Phase II glioblastoma study, the trial begins with a 1:1 randomization between the treatment and control groups. Once a statistically sufficient control group is enrolled, the randomization shifts to a 2:1 ratio, enabling more patients to receive the investigational therapy while preserving study integrity.
“We had hoped to do the trial as an open-label study,” said Hartenbach. “But feedback on our Phase I data was that it looked almost too good, so we needed the rigor of a control arm to validate it.”
The company is also collaborating with advocacy and academic groups to develop external control datasets that could support future studies. In rare or aggressive cancers, building external controls is increasingly viewed as a way to reduce the number of patients randomized to placebo or standard of care, particularly when outcomes are poor.
In its pancreatic cancer trial, Diakonos redesigned the treatment window to optimize immune function. Rather than administering therapy after adjuvant chemotherapy — when patients are immunosuppressed — the company now delivers the dendritic cell product in the interval between surgical resection and chemotherapy.
“That window was underutilized,” Hartenbach noted. “By moving treatment earlier, we think we can improve outcomes while reducing the burden on patients.”
Simplified Manufacturing, Expanded Access
Unlike CAR T-cell therapies, which require genetic engineering and weeks-long expansion processes, Diakonos’s manufacturing model is more straightforward. Monocytes are collected through leukapheresis, differentiated into dendritic cells and exposed to tumor lysate and mRNA without the use of viral vectors.
Because there is no need for lymphodepleting preconditioning or inpatient care, the therapy may be suitable for older or frailer patients who would not otherwise be eligible for cell therapy.
“It’s still personalized, but it’s significantly less complicated than other cell therapies,” said Hartenbach.
“That gives us flexibility in who we can treat and how quickly we can scale.”
This simplicity has helped Diakonos maintain lean operations.
With a team of just 20 employees, the company is conducting multiple clinical trials while expanding its manufacturing and regulatory capacity. A recently closed $20 million Simple Agreements for Future Equity (SAFE) round has funded these efforts, and a larger Series A raise is expected later this year.
Embedding Patient-Centric Values
For Diakonos, patient centricity is more than a talking point.
The company’s name — derived from the Greek word “to serve” — reflects a commitment to minimizing treatment burden and maximizing quality of life. The therapy avoids harsh side effects and complex hospital-based regimens, and the company is actively listening to feedback from trial participants.
One glioblastoma patient from the Phase I trial has remained progression-free for more than three years and has returned to an active life.
“She’s playing tennis and spending time with her grandkids,” said Hartenbach. “That’s incredibly motivating for the team.”
While anecdotes aren’t substitutes for data, they reinforce the potential value of therapies that may not only prolong survival but also preserve patient independence and dignity.
Preparing for Regulatory Engagement and Biomarker Development
As the platform matures, Diakonos is beginning to incorporate additional endpoints into its trials, including Response Evaluation Criteria in Solid Tumors (RECIST)-based response rates and progression-free survival, particularly in the upcoming melanoma study. The company’s approach does not require pre-selecting patients based on biomarkers — a benefit of using the full tumor antigen profile — but traditional metrics remain essential for regulatory submissions.
“We’re letting the dendritic cells do the hard work,” said Hartenbach. “That simplifies patient selection, but doesn’t mean we avoid rigorous evaluation.”
Staying Mission-Focused in a High-Risk Industry
As Diakonos moves toward later-stage development, its leadership remains grounded in the realities of biotech. The industry is full of failure, Hartenbach noted — not for lack of effort, but because of the complexity of the science. That’s why conviction and mission alignment are key.
“You have to absolutely believe in what you’re doing. And as you build your team, transparency is everything. Talent alone isn’t enough — you need the right people for the challenge ahead.”
— Jay Hartenbach
Diakonos Oncology’s strategy reflects a combination of scientific rigour, operational efficiency and patient-first thinking. With early signals of clinical benefit and an expanding pipeline of tough-to-treat cancers, its dendritic cell platform could offer a new approach to immunotherapy where it’s needed most.











Join or login to leave a comment
JOIN LOGIN